In laboratory diagnostics, there are various parameters available for assessing the renal function that provide a good representation of the glomerular filtration rate (GFR).
-
Creatinine
-
Symmetric dimethyl-arginine (SDMA)
-
Urine-specific gravity (USG)
-
Protein/creatinine ration (U-P/C)
| pre-renal | renal | postrenal | |
| creatinine | ↑↓ | ↑ | ↑ |
| SDMA | ↑ | ||
| USG | ↑↓ | ↑↓ | |
| U-P/C | ↑ | ↑ | ↑ |
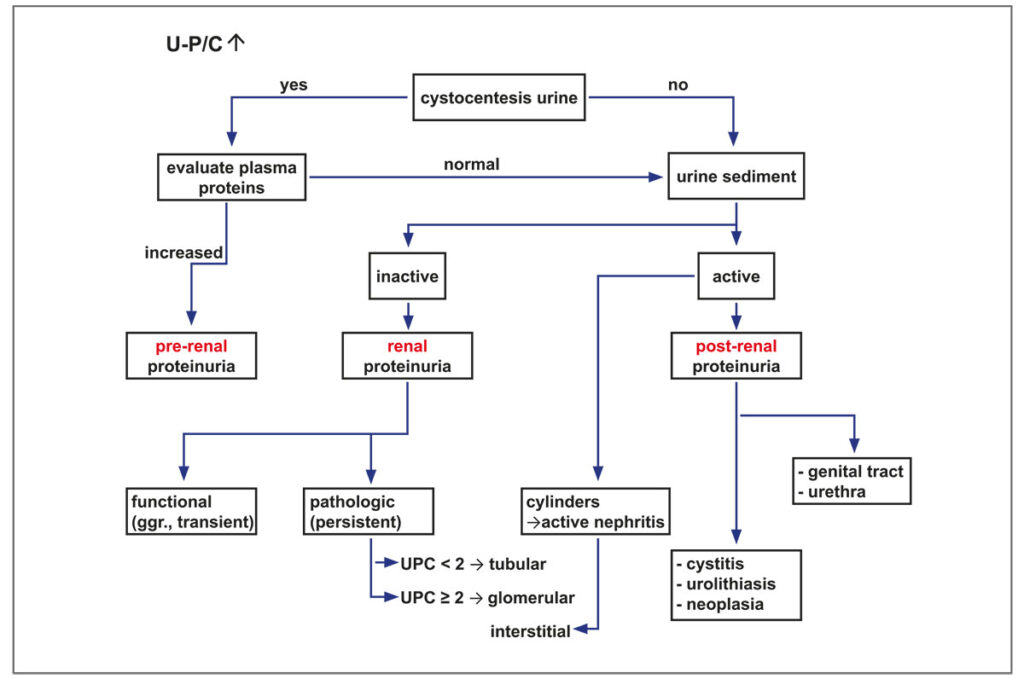
- Causes for increased U-P/C in urine.
Measurement of GFR is the gold standard for determining the filtrative and resorptive capacity in chronic renal insufficiencies. In veterinary diagnostics, it had been determined by creatinine or inulin clearance for a long time. Because of the unavailability of creatinine and inulin, however, these tests can no longer be performed.
Creatinine concentration in the serum represents the glomerular renal function with good specificity but at the same time with low sensitivity in the early stages of damage. Creatinine should be evaluated cautiously when assessing the renal function as it is prerenally influenced by several physiological factors (age, muscle mass, breed, feeding, hydration status). Postrenally, an obstruction of the urinary tract can lead to a stasis-induced increase. To assess the renal function, a primary, slight increase should be confirmed by repeated measurement. In general, a simultaneous urinalysis is always recommended. Preanalytically, haemolysis, lipidaemia or icterus impair the measurement of creatinine concentration.
Urea is a reliable parameter for assessing the glomerular renal function. However, serum concentration is subject to many pre- and postrenal influences. Urea is synthesised in the liver during amino acid degradation. It is excreted glomerularly and proportionately reabsorbed tubularly. Prerenally, urea concentration in the serum may increase due to food intake, catabolic metabolism and endocrinopathies such as Cushing’s disease or diabetes mellitus, and in case of hepatopathies with impaired function, it may decrease. Postrenally, urinary flow disorders lead to increased levels in the serum.
Another serum parameter used to assess renal function is SDMA. It is a non-proteinogenic amino acid that is produced during protein degradation. More than 90% of SDMA is glomerularly filtered and renally eliminated. In the early stages of glomerular nephropathy, SDMA is currently the most sensitive diagnostic parameter, as it already increases if GFR is reduced by 30% (creatinine only increases from 70% onwards). Thus, the isolated increase in SDMA concentration is a first indication of the onset of renal insufficiency. In patients with chronic renal insufficiency, who are often cachectic, renal function can further be monitored independent of muscle mass by measuring the SDMA concentration.
Compared to creatinine, urine specific gravity (USG) is a sensitive parameter as well and is the first to increase in case of renal insufficiency. Affected kidneys lose the ability to concentrate urine. The patient’s hydration status must be taken into account. Decreased USG alone is not specific for impaired renal function. Again, repeated measurement of several urine samples throughout the day is important for evaluation. Only a persistently low USG can be considered a pathological finding.
- Hypersthenuria (dog: > 1.030, cat: > 1.035): No indication of impaired renal function. Possibly other underlying disease.
- Normosthenuria (dog: 1.013 – 1.029, cat: 1.013 – 1.034): Normal renal function. Concurrent persistent azotaemia or proteinuria may indicate partial loss of nephrons.
- Isosthenuria (1.008 – 1.012): The USG of the urine corresponds to that of the ultrafiltrate. In case of concurrent azotaemia, this may indicate renal insufficiency in an advanced stage or nonrenal influences on the USG: hydration status, medication, hormonal influences (e.g. ADH), electrolyte changes, hepatic dysfunction, bacterial infections (e.g. E. coli), way of feeding (e.g. protein content, salt content).
- Hyposthenuria (< 1.008): independent of renal function (e.g. diabetes insipidus). The evaluation of the protein excretion in the urine should always be performed in conjunction with the evaluation of the USG and a urinary status/sediment (Figure).
For quantifying proteinuria, the protein/creatinine ratio UP/C is determined in urine. After IRIS staging, the UP/C reflects the extent of renal protein loss.
At times, low-grade proteinuria is physiological, whereas pathological proteinuria persists (medium to highgrade). Causes for extrarenal, high-grade proteinuria are listed in the table below.
| DOG | CAT | |||
| U-P/C < 0.2 | U-P/C < 0.2 | no proteinuria | ||
| U-P/C 0.2 – 0.5 | U-P/C 0.2 – 0.4 | borderline proteinuria | ||
| U-P/C > 0.5 | U-P/C > 0.4 | proteinuria | ||
Causes for extra-renal, high-grade proteinuria
| Infectious diseases | Immune-mediated diseases | Neoplasia | Glomerulopathies (GP) |
| • leishmaniosis
• ehrlichiosis |
• systemic lupus
• IgA nephropathy |
• monoclonal gammopathy
• plasmocytoma |
• amyloidosis
• membranous GP • membrano-proliferative GP |
However, medium or low-grade proteinuria does not exclude nephropathy. It is therefore important to localise proteinuria to distinguish between physiological, temporary proteinuria (exertion, exposure to heat or cold, stress) and pathological proteinuria. Pathologically, glomerular as well as tubular or interstitial proteinuria can occur.
This can be diagnostically differentiated by urinary electrophoresis.
In male dogs, retrograde ejaculation can also cause proteinuria. There are not always sperms in the urine samples, which makes diagnosis difficult.
Diseases leading to a restriction of tubular renal function include cystinuria and Fanconi syndrome.
Both diseases are characterised by an increased excretion of amino acids in the urine. Both diseases may or may not be associated with an increase in UP/C.
Cystinuria is a genetic amino acid transport disorder in dogs and rarely in cats. The mutation is known in the breeds Australian Cattle Dog, Continental Bulldog, English Bulldog, French Bulldog, Labrador Retriever, Landseer, Mastiff, Newfoundland, Olde English Bulldogge and Miniature Pinscher. The patients lack a transmembrane transport protein in the epithelial cells of the small intestine and in the proximal tubular cells that reabsorbs cystine, ornithine, lysine and arginine. The excretion of cystine via the kidney is increased to the rate of 20 to 30 times the norm, while the concentration in the blood remains unchanged. Cystine is poorly solublein normal urinary pH. If the concentration is ≥ 300 mg/l or more, crystals precipitate in the urine. Often, calculi are formed. Diagnosis is made by genetic testing or, in animals in which the mutation is not known, by determining the concentration of amino acids in the urine – the COLA test.
In clinically affected animals, cystine crystals are found in the sediment.
Fanconi syndrome is a genetic disease that occurs in Basenjis. Idiopathically, it has been identified in Norwegian Elkhound, Labrador Retriever, Sheltie and Miniature Schnauzer. Acquired Fanconi syndrome is caused by the toxic effects of certain medication, heavy metal poisoning or feeding of disproportionately large amounts of dried meat. Dried meat causes a deficit in tubular reabsorption of glucose, amino acids and bicarbonate. The result is renal tubular acidosis. The clinical picture often corresponds to that of patients with glomerular renal insufficiency with apathy, inappetence, PU/PD, weight loss, dehydration, weakness, vomitus.
In the blood test, neutrophilia with a mild left shift, changes in the clinical chemical parameters and in the urinary status/sediment are noticeable (see Table). The definite diagnosis is made by quantitative determination of the amino acids threonine, glutamine, proline, glycine and alanine in the urine with simultaneous semiquantitative measurement of glucose excretion.
| Cystinuria | Fanconi syndrome | Diabetes | |
| Urine | U-P/C↑≈, cystine crystals, COLA↑ | U-P/C↑≈, COLA↑≈, glucose↑, amino acids | U-P/C↑≈, glucose↑, |
| Serum | normal | Cl ↑, glucose ≈↓, K↓, PO4↓, Na↓, fructosamines↓, urea↑, creatinine↑, aldosterone↑, ALT↑ | glucose↑, fructosamines↑, Na↑↓, K↓↑, PO4↓ |