Dangers from rodenticides and dead rodents
Rodenticides (‘rat poisons’) are repeatedly the cause of life-threatening poisoning in dogs and cats. Primary poisoning can occur through the direct ingestion of poisoned bait, e.g. if it has been improperly placed in an open area for ‘pest control’ (Fig. 1a). Secondary poisoning can result from the ingestion of poisoned rodents (Fig. 1b). The ingestion of the bait or the dead rodents is often not directly observed by the animal owners or it is often not known what type of poison is involved. If the animals are presented to the practice with suspected poisoning, the ‘cat-and-mouse game’ often begins with the search for the cause of the poisoning symptoms or the poison causing it.
Two currently important rodenticides and classes are presented below:
α-Chloralose
The use of this substance, which was originally used as a narcotic and later also as an avicide (poison against birds), has risen significantly in Europe in recent years (Dijkman et al. 2023). The sale of bait material containing the poison α-chloralose is poorly regulated, making it easy and therefore common to obtain through online sales.
Symptoms of poisoning with α-chloralose are essentially based on the depressive effect of the substance on the central nervous system (CNS).
Depending on the dose, seizures and convulsions, particular susceptibility to external stimuli (hyperreflexia), hypersecretion, depression, somnolence, bradypnoea and even dsypnoea may occur. Hypothermia is also common, as the poison also impairs thermoregulation through the CNS (toxic principle particularly effective against wild rodents and birds). The occurrence of neurological symptoms combined with hypothermia can confirm the suspicion of poisoning with α-chloralose.
Poisoning with α-chloralose must be counteracted by symptomatic therapy, in particular by stabilising measures for circulation, respiration and body temperature. Direct detection of the toxin is possible from serum or urine. Decontamination should be considered if the ingestion occurred within the last few hours.
-
Fig. 1a): Sources of danger for dogs and cats – Poisoned bait
Image source: envatoelements
-
Fig. 1b): Sources of danger for dogs and cats – Poisoned rodent
Image source: envatoelements
-
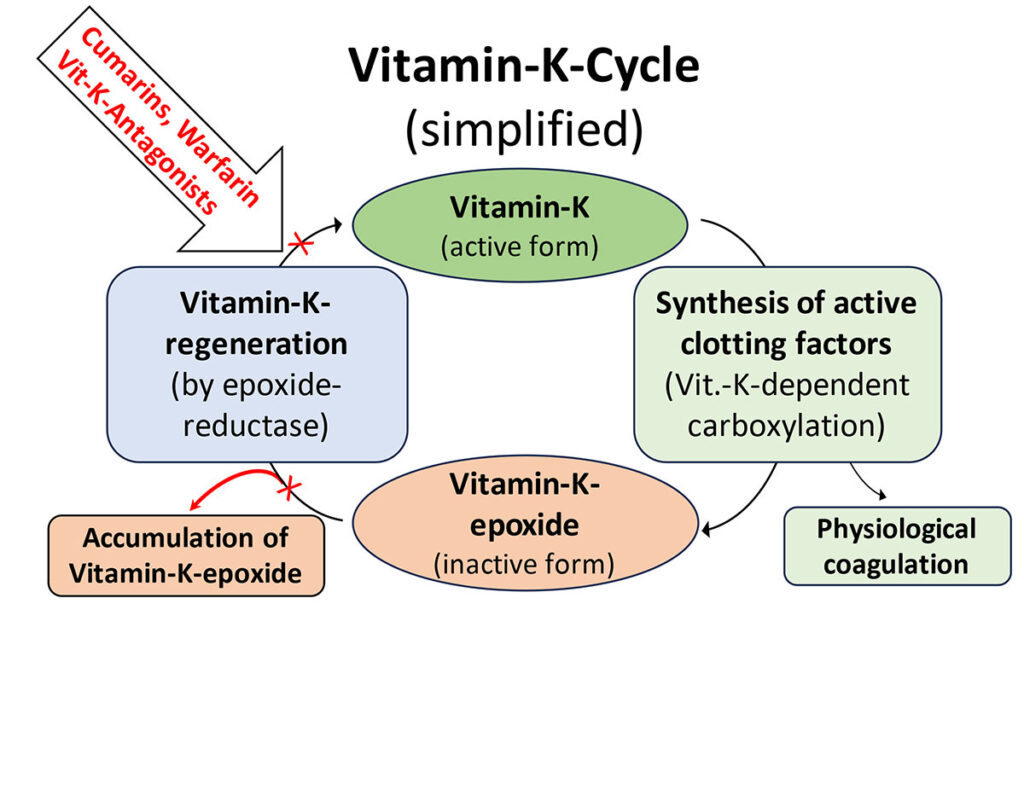
Fig. 2: Vitamin-K-cycle (simplified)
Image source: Laboklin
Coumarin derivatives (vitamin-K-antagonists)
Rodenticides that indirectly target the vitamin-K-dependent blood coagulation factors (vitamin-K antagonists) are frequently used. Derived from coumarin, which occurs naturally in fungi and plants (keyword: sweet clover disease), a large number of so-called coumarin derivatives have been developed.
The first generation of these active substances includes the medication known as warfarin. The duration of action of the first-generation substances was still short with low potency, which allowed them to be used as a controllable drug or rodenticide.
Second-generation substances, such as brodifacoum and coumatetralyl, which are frequently used against rodents today, were developed with the particular aim of being able to use the substances even more successfully as rodenticides. These substances are particularly dangerous as they have been ‘optimised’ for their potency and unfortunately also for the slowest possible metabolism by the organism.
Figure 2 shows the simplified description of how vitamin-K antagonists unfold their devastating effect on the blood coagulation factors of animals. Under physiological conditions, vitamin-K is constantly ‘consumed’ in the liver to form active coagulation factors (e.g. factor II, VII, IX, X as well as protein C and S) and converted to the inactive form vitamin-K-epoxide.
Under physiological conditions, vitamin-K-epoxide is enzymatically converted back to vitamin-K in the liver by epoxide reductase, allowing it to be used again for the formation of active coagulation factors and only being detectable in the serum in a concentration well below 10 ng/ml.
All coumarin derivatives attack this cycle. They inhibit epoxide reductase and therefore prevent ‘regeneration’ of the inactive vitamin-K-epoxide to active vitamin-K. This explains the often delayed onset of clinical signs of poisoning, as active coagulation factors and vitamin-K are still present after ingestion of the toxins. However, both are consumed at different rates, depending on the half-life of the various factors and the initial situation of the affected animal. As soon as the active coagulation factors are depleted, typical symptoms of severe coagulopathies occur, such as bleeding on mucous membranes and in the mediastinum, abdomen and thorax, etc. Coagulation parameters are severely altered, although the platelet count may initially appear normal.
Laboratory testing of coagulation parameters is urgently indicated in cases of suspected poisoning with coumarin derivatives. If there is reasonable suspicion of ingestion of such toxins, treatment with vitamin-K as an ‘antidote’ is indicated. Supplemented vitamin-K enables the liver to produce active coagulation factors again. An initial administration of up to 10 mg/kg bw intravenously is indicated in severe cases, with a switch to vitamin-K orally if clinical improvement is observed. We refer here to a recently published article on this topic (Frommeyer and Mischke, 2024).
Due to their high potency, i.e. very low concentration in plasma, and the additional problem that the effect of the substances in the liver can last for a long time, even if the active substance itself is no longer detectable in plasma, the direct detection of coumarin derivatives is generally of little help in clinical cases.
Stanford University demonstrated a long time ago that an increase in vitamin-K-epoxide in serum (Carlisle et al. 1981) can provide direct conclusions about the activity of vitamin-K antagonists in the liver. We were able to establish a detection method for vitamin-K-epoxide from serum by LC-MS/MS and thus a functional detection of coumarin activity.
We are pleased to be able to offer you a serum test for coumarin activity (level of vitamin-K-epoxide). This can functionally confirm intoxication with coumarin derivatives (increase in vitamin-K-epoxide). The analysis is possible without having to interrupt the vitamin K-therapy. We can also provide you with information on when the toxin is no longer active in the liver, i.e. when vitamin-K therapy can be safely stopped (decrease in vitamin-K-epoxide).
Dr. Simon Franz Müller
Range of services
- 0548 α-Chloralose
- 0511 Coumarin activity (vitamin-K-epoxide)
- 0595 Coagulation