The umbrella term erythema multiforme (EM) complex covers a group of rare immunemediated diseases in dogs and cats, in which cytotoxic T-cell-mediated destruction of epidermal keratinocytes leads to vesicles, detachments, and ulcers in the skin and cutaneous mucous membranes.
The classification of these diseases is complex and sometimes controversial. However, a distinction is made between EM minor, EM major, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), depending on the extent of the skin and mucosal surface involved. The exact pathogenesis of EM in pets is unclear, but the activation of T lymphocytes by viral antigens or drugs is suspected, resulting in the recognition and destruction of keratinocytes.
EM in human medicine
In human medicine, EM (minor) was first described in 1860 by Ferdinand von Hebra. This condition is typically a self-limiting acute skin disease, characterised by ‘target lesions’ that primarily affect the limbs. While EM in humans generally has an infectious aetiology, such as Herpes simplex or Mycoplasma pneumoniae, SJS/TEN is most often the result of an adverse drug. EM minor usually has a mild clinical course.
In contrast, SJS/TEN and TEN are dermatological emergencies that necessitate extensive, intensive medical treatment.
In 1993, an internationally recognised standardised classification was developed to objectively differentiate between TEN, SJS, and EM (see Table 1). In human medicine, there are two internationally recognised guidelines for the treatment of SJS; however, no such document yet exists for EM. For SJS/TEN, the primary focus is on discontinuing the causative medication and providing intensive supportive therapy, especially in patients with extensive skin detachment. The use of immunosuppressive drugs remains controversial.
In particular, for intubated patients with central catheters, it involves a trade-off between an increased risk of sepsis and the potential benefit of preventing further progression of skin detachment. However, literature suggests that treatment with ciclosporins may reduce both the mortality rate and the progression of skin detachment.
In both human and veterinary medicine, TEN is a serious disease associated with a high mortality rate, even with intensive therapy. In human medicine, a prognostic assessment of mortality risk can be made using a scoring system based on various parameters. A low score (0-1) correlates with a relatively low mortality rate of 3.2%, while a score greater than 4 indicates a mortality risk of over 90% (see Table 2). Some prognostic factors (e.g., heart rate, urea) have yet to be evaluated in veterinary medicine. Interestingly, in human medicine, paediatric patients exhibit a significantly lower mortality rate compared to adults. However, it can generally be assumed that mortality in dogs and cats correlates with the extent of the affected body surface area.
-
Fig. 1: Initial skin detachment in the area of the nose and muzzle, along with target-like eruptions on the lower chest
Image source: Jan Declercq
-
Fig. 2: Progression to extensive skin detachments on the face and body due to prolonged cephalosporin therapy
Image source: Jan Declercq
-
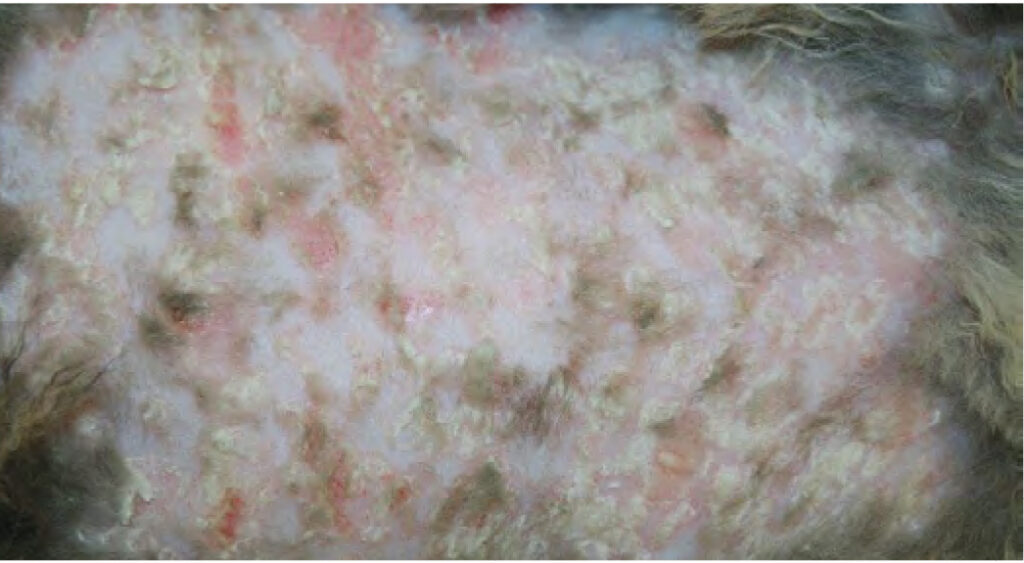
Fig. 3: Skin lesions on the ventral abdomen of a cat with EM associated with FHV-1 infection
Image source: Jan Declercq
-
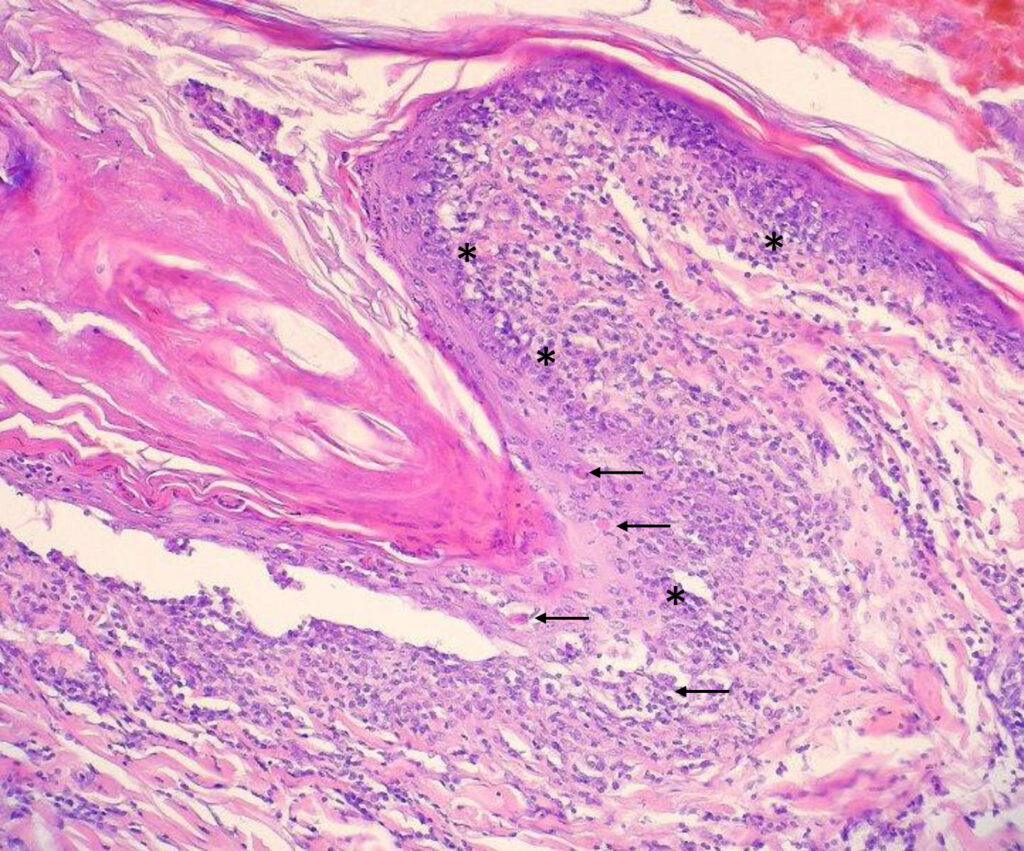
Fig. 4: Lymphohistiocytic border zone dermatitis with keratinocyte apoptosis and lymphocytic satelliteosis → apoptotic keratinocytes, * dermoepidermal junction masked by inflammatory cells
Image source: Laboklin
Table 1: Consensus definition of severe blistering skin reactions (human medicine)
| Criteria | EM minor | EM major | SJS/TEN overlap | TEN with maculae | TEN without maculae |
| Skin detachment | <10% | <10% | 10-30% | >30% | >10% |
| Target lesions | typical or atypical | atypical | atypical | atypical | atypical |
| Raised lesions | yes | no | no | no | no |
| Distribution | primarily on trunk | primarily on limbs | primarily on limbs | primarily on limbs | primarily on limbs |
| Progression to TEN | no | possible | possible/likely | – | – |
Table 2: Scoring system by type of score (human medicine)
| Criteria | Points |
| Age >40 | 1 |
| Heart rate >120 | 1 |
| Underlying malignant tumour disease | 1 |
| Skin detachment >10% on the first day | 1 |
| Urea >10 mmol/L | 1 |
| Bicarbonate <20 mmol/L | 1 |
| Serum glucose >14 mmol/l | 1 |
| Scorten score | Risk of mortality |
| 0-1 | 3,2% |
| 2 | 12,1% |
| 4 | 35,8% |
| 4 | 58,3% |
| >4 | >90% |
EM for cats and dogs
EM is a rare skin disease that affects 0.4% of canine dermatological patients and 0.11% of feline patients, according to a study conducted at an American university hospital. The incidence of SJS/TEN and TEN remains unknown. In humans, a diagnosis of EM requires evidence of typical or atypical target lesions; however, classic target lesions are observed in only a minority of cases in dogs and cats. EM presents with variable clinical features but is often characterised by bilaterally symmetrical maculopapular eruptions that primarily affect the axilla and groin, as well as the oral mucosa, pinna, and footpads.
These lesions are painful but generally non-pruritic. While EM is strongly associated with herpes simplex virus (HSV) infections in humans, adverse drug reactions appear to be the primary cause in veterinary medicine.
Various medications, including antibiotics (e.g., chloramphenicol, enrofloxacin), antiparasitics (e.g., ivermectin, moxidectin, levamisole), and even shampoos (e.g., benzoyl peroxide), can trigger EM in dogs (see case study Figures 1 and 2). Known infectious triggers include anal sac inflammation, pneumocystis infections, as well as herpes and parvovirus infections. In cats, EM may be associated with feline herpesvirus infection (FHV-1, Figure 3) or adverse drug reactions. Additionally, neoplasia might be an underlying cause, and thymoma-associated exfoliative dermatitis may represent a form of EM in cats. In a significant proportion of cases, no identifiable trigger is found, and the disease is considered idiopathic.
Since target lesions, considered pathognomonic in human medicine, often do not appear in veterinary medicine, diagnosing EM requires a thorough medical history, including previous drug therapy, as well as clinical findings and pathohistological examination.
The pathohistological picture of EM is characterised by transepidermal keratinocyte apoptosis with lymphocytic satellitosis, accompanied by lymphohistiocytic interface dermatitis and ulceration (see Figure 4).
The treatment of diseases within the EM complex depends primarily on the severity and extent of the changes. Mild cases of EM minor can be self-limiting, whereas EM major, SJS/ TEN, and TEN often require intensive supportive therapy. In general, efforts should be made to identify and, if possible, eliminate the trigger, such as discontinuing any medication suspected of causing an adverse reaction. If the trigger can be eliminated, the skin lesions in EM patients resulting from an adverse drug reaction typically heal over several weeks without the need for immunomodulatory therapy. If the cause of EM cannot be identified, or if the severity of the disease warrants it, immunosuppressants such as glucocorticoids, azathioprine, and ciclosporins may be used. Intravenous immunoglobulins (IVIG) are another, albeit cost-intensive, therapy option. However, recent data from human medicine indicate that IVIG has no significant effect on the mortality rate of TEN, at least in adult patients.
The treatment of SJS/TEN overlap and TEN is based on three fundamental principles:
- Discontinuation of medications suspected to be the trigger or addressing the underlying cause, such as bacterial infections.
- Correction of fluid and electrolyte imbalances.
- Prevention of wound infections and sepsis due to skin detachment and ulcers.
Additionally, efforts should be made to minimise the progression of skin detachments through immunomodulatory therapy. This aspect of treatment remains controversial, as such therapy may increase the risk of sepsis. Data from human medicine indicate that ciclosporins can reduce mortality in patients with TEN, likely due to their inhibition of T-cell function via the calcineurin phosphatase pathway.
Diseases of the EM complex present significant diagnostic and therapeutic challenges, where pathohistological examination is crucial for accurate diagnosis. Our clinical and dermatopathological team is available to assist with complex skin cases.
Ines Hoffmann