As with all skin problems, a thorough history is the most critical tool to arrive at a diagnosis in the cat. The preliminary report at the initial consultation takes a good 20 minutes and often already represents up to 70 – 90% of the diagnosis. It is often easier to reach a tentative diagnosis with an owner without a cat than with a cat without an owner.
The anamnesis for the work-up of a skin problem in the cat contains the same questions as in any other animal species and begins with signalment. Questions such as “Do other in contact animals or humans have skin lesions?” must never be forgotten, as they can provide important clues to a contagious disease such as dermatophytosis or ectoparasitic diseases. It is also essential to ask whether the cat is free-roaming because with a free-roaming cat, for example, a strict elimination diet is more or less impossible. Changes in the family environment (new baby, moving house, changes in the family members, renovation of the flat) can lead to marking in sensitive cats and psychogenic excessive grooming behaviour, which may result in alopecia and other skin lesions.
Information on pruritus is often misleading, especially in cats. Many cats do not show their pruritus in front of the owner; they hide to lick themselves, and the owner is convinced that the cat has spontaneously lost its hair. Inquiring about the occurrence of hair vomiting or problems with hairballs may help to identify excessive grooming behaviour. In addition, some cats may be found to have hair between their teeth when the mouth is inspected.
It is also important to differentiate whether the hair has fallen out (the whole hair, including the root, is missing) or whether the hair has broken off (the hair root is still present). In the first case, there is a disease with hair loss, either of hormonal origin (relatively rare in cats) or follicular infections such as dermatophytosis. In these cases, the hair is easily depilated. If the hair is broken off (self-induced alopecia), pruritus is usually present, the cat licks itself, and the hairs break off in the process. The problem is that owners hardly ever observe their cat licking itself, and in the anamnesis, they swear that the hair has fallen out. There are several ways to convince oneself and the owners that the alopecia is self-induced: use a magnifying glass to see the broken hair shafts or take a skin fold and see the hair stubble at the edge. A trichography can also be performed. Place hair samples from the lesion on a slide with a drop of oil and examine them under the microscope. The tip of the hair usually is nicely pointed; however, if the hair tip is blunt, then the hair has broken off by grooming (Fig. 1). The presence of fractures confirms a self-induced licking alopecia.
Cats are not small dogs!
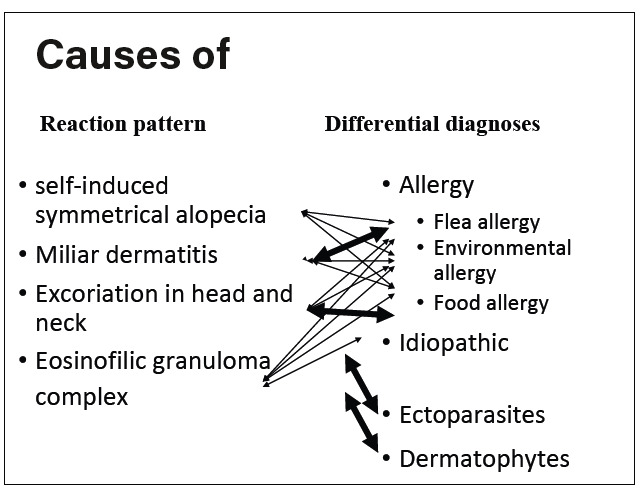
It is necessary to distinguish between pruritic and non-pruritic skin diseases, allergic and nonallergic diseases, and the differential diagnoses of each dermatological reaction pattern. Cats often react with different skin reaction patterns, which have many differential diagnoses, at the same time, the same disease can manifest with a variety of reaction patterns (Fig. 8). Therefore, it is often more challenging to get to the bottom of the cause of the skin problem in cats than, for example, in dogs.
Regarding the aetiology of pruritus in cats, the following causes are possible including ectoparasites (Notoedres, Otodectes, Cheyletiella, Demodex, lice, hair lice, Trombicula), allergies and infectious diseases (bacterial infections, dermatophytosis, which,are usually not primarily pruritic). Pruritus may also occur as an associated sign in viral diseases (herpesvirus, poxvirus), immune-mediated diseases (pemphigus foliaceus, drug reactions, mural folliculitis, sebaceous adenitis) and cutaneous neoplasms (e.g. lymphoma).
As discussed alopecia is a common lesion in cats which is often mistakenly dubbed as hair loss. In most cases, pruritus causes the cat to lick and pluck out its hair. Symmetrical alopecia is commonly produced by the cat itself and is not hair loss in the true sense of the word; pruritus of allergic, ectoparasitic or psychogenic origin is a possible cause. On the other hand, alopecia is primary in dermatophytosis, demodicosis, alopecia areata, pyoderma and paraneoplastic alopecia, in which the skin also appears smooth and shiny.
Skin lesions in the cat are often reaction patterns, but they do not represent specific diseases.
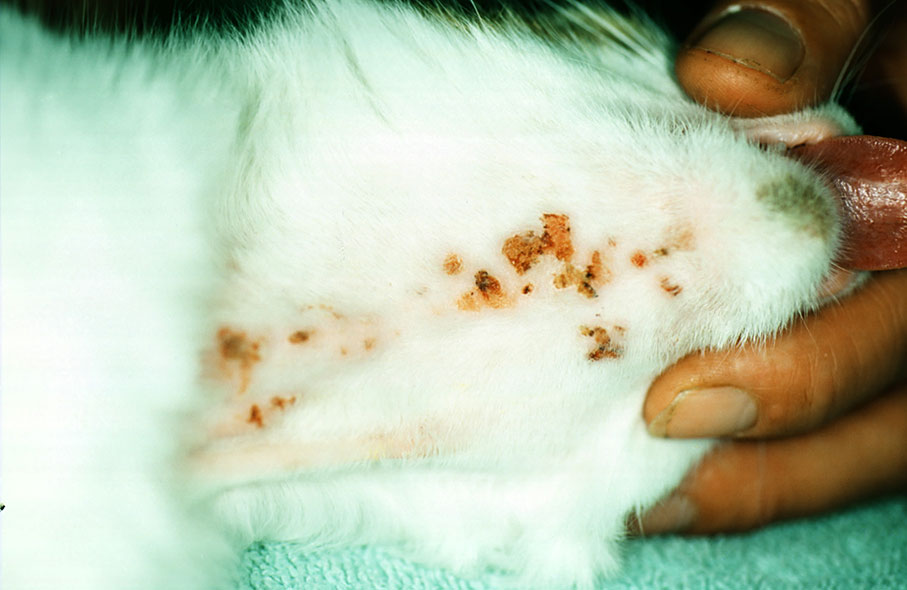
1. Miliary dermatitis: many small miliary scabs are scattered over the body; they are felt rather than seen. This reaction pattern is often seen in flea allergy, but all other allergies, ectoparasites and dermatophytoses can also trigger it (Fig. 2).
2. Self-induced ulcers of the head and neck: as the name suggests, these are self-inflicted injuries to the head and neck of the cat. It is not uncommon for the cat to scratch so severely that it injures itself and causes deep, bleeding ulcers. This reaction pattern is often seen in food allergies but also other allergies, ectoparasites and dermatophytoses (Fig. 3).
3. Self-induced symmetrical alopecia: the difference between hair loss and self-injury has already been discussed above. In this reaction pattern, patches of alopecia, sometimes symmetrical, appear on various body parts. Areas usually affected are the abdomen, limbs and occasionally the back. The skin is generally free of other lesions (Fig. 4).
4. Eosinophilic granuloma complex (EGC):
A. Eosinophilic ulcer (indolent/rodent ulcer): the lesion is ulcerated and necrotic, located on one or both sides of the upper lip and is usually not pruritic or painful. Eosinophilia is rarely present in the blood or tissues (Fig. 5).
B. Eosinophilic plaque: a pruritic, welldemarcated, slightly raised, rounded, exudative lesion that usually occurs on hindlimbs, abdomen or within the groin area (Fig. 6). Secondary bacterial infections aggravate the pruritus. Eosinophilic granulocytes are found in cytology.
C. Eosinophilic granuloma. This form has different presentations and locations.
a. Linear granuloma. An elongated, hard, palpable elevation on the caudal hindlimb.
Rarely on the chin, corner of the mouth, pinna, and paws (Fig. 7).
b. Pharyngeal granuloma: may be allergic or idiopathic (Fig. 5).
c. Eosinophilic granuloma of the chin, also called “fat chin”.
The reaction patterns mentioned above can occur together in the most diverse combinations. The differential diagnoses apply to all reaction patterns: allergic diseases (to flea bites, food and environmental allergens or feline atopic skin syndrome (FASS)), ectoparasitic diseases and dermatophytosis (Fig. 8). The cause must be identified and treated accordingly. If the cause is allergic, symptomatic treatment with glucocorticoids, cyclosporine or antihistamines should be applied. Indolent ulcers, eosinophilic plaques, miliary dermatitis and self-induced head and neck ulcers experience improvement of secondary infection with antibiotic treatment.
Unquestionably, the best therapy for allergic processes is allergen avoidance. It is possible in flea bite allergy dermatitis (continuous flea treatment of the affected animal and all accompanying animals) and food allergy (elimination diet, provocation diet and lifelong diet with tolerated components). In the case of environmental allergy (pollen, house dust and storage mites, moulds), allergen avoidance would not only be highly time-consuming and expensive but, in most cases, not even possible. For many cats, allergen-specific immunotherapy (ASIT, hyposensitization) offers an effective treatment option; the success rate is between 60-78%. ASIT is recommended as a lifelong therapy, as experience shows that recurrence is often expected within 1-2 years after treatment discontinuation.
-
Fig. 1: Tapered hairs and broken hairs are evidence of licking
Photo credits: Dr Regina Wagner
-
Fig. 2: Miliary Dermatitis
Photo credits: Dr Regina Wagner
-
Fig. 3: Self-induced ulcers in the head
Photo credits: Dr Regina Wagner
-
Fig. 4: Self-induced alopecia
Photo credits: Dr Regina Wagner
-
Fig. 5: Eosinophilic ulcer and pharyngeal granuloma
Photo credits: Dr Regina Wagner
-
Fig. 6: Eosinophilic plaque
Photo credits: Dr Regina Wagner
-
Fig. 7: Linear granuloma
Photo credits: Dr Regina Wagner
-
Fig. 8: Differential diagnoses of feline reaction patterns
Graphic credits: Dr Regina Wagner
Dermatophytosis, cheyletiellosis, otoacariosis, D. gatoi demodicosis and lice infestations should also be included in the differential diagnosis of the feline skin reaction pattern lesions. Almost all dermatophyte infections in cats are caused by Microsporum canis. Not every cat shows lesions as there are asymptomatic carriers who act as a reservoir. Dermatophyte culture or PCR should be performed to diagnose the disease. To detect asymptomatic carriers, the coat is sampled using the so-called McKenzie method by brushing the animal with a sterile toothbrush or sterile piece of carpet. If a member of the family has compatible skin lesions (especially children, elderly or immunocompromised persons), the suspicion of dermatophytosis is high. In the case of ectoparasites, cheyletiellosis is an important differential diagnosis. These mites are species-specific, but cross-infestations between dogs, cats and rabbits can also occur. Typical lesions, in addition to feline skin reaction patterns, are white dry scales with or without pruritus. Otodectes mites should also be included in the differential diagnosis of pruritus reaction patterns in the cat, as even ectopic parasitism has been described.
Infections with Demodex gatoi may present a clinical picture similar to that of notoedric mange or feline atopic syndrome: head pruritus with crusting and self-injury. As this mite lives very superficially, it is diagnosed by superficial skin scraping (unlike other Demodex mites, which are diagnosed by deep skin scraping). However, due to intensive licking, the scraping may be falsely negative (but it can sometimes be found in faeces), in which case it would be diagnosed by response to treatment.
Although infestations with Felicola subrostratus (the main cat louse) are now rare, they should be considered in the differential diagnosis of feline reaction patterns. It mainly affects young, debilitated or stray animals and presents with variable pruritus, excoriations and seborrhoea.
Dr Regina Wagner