Alopecia or pathological hair loss is a frequent reason for consultation with dermatological patients, a variety of skin diseases in dogs can cause impairment of hair growth. Shedding is a physiological process and occurs twice a year in most dogs, but there is also a breed-specific rhythm. The anagen phase (growth phase) lasts a very long time in the poodle, for example, and is shorter in other breeds such as sheepdogs, retrievers and boxers. Reduced or arrest of the anagen phase or increased hair loss in the resting phase/telogen phase of the hair cycle can lead to alopecia in dogs.
Alopecia can be caused by many processes or diseases such as endocrinopathies (hypothyroidism, hyperadrenocorticism, hyperestrogenism, Sertoli cell tumour), drugs (chemotherapy, drug reactions), parasites (demodicosis), infections (pyoderma, dermatophytes), immune-mediated diseases (pemphigus foliaceus, sebaceous adenitis), congenital disorders (follicular dysplasia), trauma, telogen or anagen effluvium and alopecia X.
A detailed history is required to make a differential diagnosis, e.g. sudden alopecia after chemotherapy suggests anagen effluvium. When a dog shows alopecia and another member of the family also has skin lesions, dermatophytosis diagnosis should be considered. The presence of pruritus is a critical anamnestic question in choosing the correct diagnostic algorithm. In general, one of the main problems is knowing which came first, alopecia or itching? Also, consider the following aspects during dermatological research:
- The symmetry of the lesions (symmetric alopecia / non-symmetric alopecia)
- The inflammatory properties of the lesions (inflammatory alopecia / non inflammatory alopecia)
Inflammatory alopecia
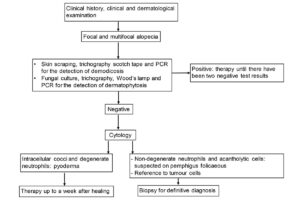
Inflammatory alopecia is the most common cause of alopecia in dogs. Alopecia can be focal or multifocal. It may be a consequence of infections or conditions affecting the hair follicle structures (e.g. immune-mediated diseases, sebaceous adenitis). Inflammatory alopecia is not symmetrical and can be primary, caused by infections of the hair follicles as a result of conditions such as demodicosis, dermatophytosis, pyoderma or can be secondary alopecia, e.g. due to scratching in allergic diseases.The diagnosis can’t be based only on clinical examination. Diagnostic tests such as cytology, deep skin scraping, scotch tape, trichography, dermatophyte culture, Wood’s lamp, PCR and biopsy could be needed according to the diagnostic algorithm (Fig. 1).
- Picture Credits: Dr Maria Christian
- Fig. 1: Diagnostic algorithm for inflammatory alopecia
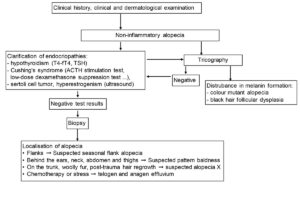
- Fig. 2: Diagnostic algorithm for non-inflammatory alopecia
Demodicosis
The abnormal multiplication of Demodex mites (Demodex canis is most commonly found however Demodex cornei and Demodex injai could also be present) in hair follicles or, rarely, in sebum glands causes demodicosis in dogs. According to the number of lesions, demodicosis is classified as localised (mild) < 4 lesions; and in generalised demodicosis (moderate to severe form) when > 4 lesions are found. Immunocompromised patients or young dogs (less than one-year-old) are predisposed to demodicosis. The classic clinical picture is a focal or multifocal to generalised inflammatory alopecia. Comedones, follicular cast and hyperpigmentation are other common lesions. Lesions are usually distributed on the face, neck, front paws, rump and trunk. Pruritus is not a primary sign, but it can occur later due to secondary infection.
Diagnosis of demodicosis requires deep skin scraping, scotch tape, trichography, PCR and/or a biopsy. The localised form is self-limiting in most patients, but generalised demodicosis can develop. Secondary infection must be ruled out by cytology. The isoxazolines (fluralaner, sarolaner, lotilaner and afoxolaner) are very effective preparations against demodicosis. Therapy should be administered until two negative skin scrapings are present one month apart.
Dermatophytosis
Dermatophytes, Microsporum canis, Nannizzia gypsea (formerly Microsporum gypseum) and Trichophyton mentagrophytes (in dogs in rural areas) cause dermatophytosis in dogs. Dermatophytosis occurs mainly in immunocompromised or young animals, especially when cats (asymptomatic carriers) live in the same household. Yorkshire terriers appear to be predisposed to Microsporum canis and Jack Russel Terrier to Trichophyton mentagrophytes. The classic lesions in dogs are focal to generalised non-symmetrical inflammatory alopecia, follicular cast, desquamation, folliculitis, furunculosis, onychomycosis and kerion (multiple or solitary nodular lesions) on the face and extremities which often occur without itching. Fungal culture and dermatophyte PCR, trichoscopy, Wood‘s lamp and sometimes a cytological examination are useful for diagnosing dermatophytosis. A zoonotic potential, especially for children and immunosuppressed people, makes therapy necessary. The most effective topical and systemic antifungal drugs against dermatophytes are imidazoles (enliconazole, itraconazole, ketoconazole, miconazole, clotrimazole). Topical and systemic therapies are necessary until complete resolution of the lesions is achieved and there are two negative fungal culture results four weeks apart.
Pyoderma
Bacterial infection of the skin rarely occurs as a primary disease in dogs, pyoderma is prevalent as a secondary condition of skin disease with allergies, parasitic infestations, endocrine diseases and keratinization disorders. Depending on the depth of the infection, pyoderma is classified into surface pyoderma (pyotraumatic dermatitis, intertrigo), superficial pyoderma (impetigo, mucocutaneous pyoderma, bacterial folliculitis) and deep pyoderma (interdigital furunculosis, pyotraumatic furunculosis, nasal furunculosis). Pyoderma appears clinically with inflammatory non-symmetrical alopecia, epidermal collarettes, exfoliative dermatitis, papules, pustules, crusts, etc. Diagnostic tests include cytology, bacterial culture and antibiogram to select the antibiotic, and in deep infection, a biopsy maybe indicated. Antiseptic preparations such as chlorhexidine shampoo are used for topical treatment. Empirical selection of cephalexin or amoxicillin-clavulanic acid, for systemic therapy, can be done in non-complex superficial infections. Treatment should be maintained for at least 3 weeks or up to a week after the lesions resolve. Bacterial culture and antibiogram are necessary in deep pyoderma, unsuccessful therapies, immunocompromised patients and when cytology shows the presence of rod bacteria.
Non-inflammatory alopecia
The causes of non-inflammatory alopecia include hormonal diseases (such as hypothyroidism, hyperadrenocorticism or Cushing‘s syndrome, hyperestrogenism, and Sertoli cell tumour) and hair follicle dystrophy/dysplasias (dilute colour alopecia) and alopecia X. Non-inflammatory alopecia usually appears symmetrical, in the absence of other skin lesions and without pruritus. But pruritus may occur if secondary infections develop (bacterial infections, Malassezia dermatitis). It is essential to obtain the initial clinical picture of skin changes and evaluate this with the clinical history and existing skin changes to make the differential diagnosis. The diagnostic tests of choice are trichography, cytology (to rule out secondary infections), laboratory tests (including specific diagnostic tests) and, if necessary, a biopsy (Fig. 2).
Hypothyroidism
Hypothyroidism is the most common cause of symmetric non-inflammatory alopecia in dogs. In addition to the classic skin changes (non-inflammatory symmetric alopecia) 60 – 80% of cases present with secondary infections. Other typical clinical signs of hypothyroidism are observed, such as weight gain, bradycardia, lethargy, apathy, infertility, disorders of the libido and hypothermia. Blood parameters such as cholesterol, ALP, ALT and creatine kinase may be elevated and there may be mild non-regenerative anaemia. Low levels of total T4 and free T4 and a simultaneous increase in TSH allow the diagnosis of hypothyroidism. Levothyroxine therapy is started with a dose of 10 μg/kg twice daily. Whenever skin lesions persist, secondary infections should be ruled out by cytology.
Hyperadrenocorticism
Hyperadrenocorticism (HAC) or Cushing‘s syndrome can occur spontaneously or iatrogenically (due to the administration of glucocorticoids) and often causes symmetrical non-inflammatory alopecia in the dog. The classic clinical signs are polyuria/polydipsia (PU/PD), polyphagia, obesity, a pendulous abdomen, muscle and skin atrophy, symmetrical alopecia, calcinosis cutis, hepatomegaly, anoestrus, etc. Demodicosis should be excluded in patients with HAC, especially in the presence of comedones. Hypercholesterolemia, increased ALT and ALP activity, decreased total T4 (due to the inhibitory effect of corticosteroids) and low urine specific gravity (<1.015) are typical laboratory findings in HAC. The specific diagnostic tests are the low-dose dexamethasone suppression test (LDDST, gold standard for spontaneous HAC), ACTH stimulation test (diagnosis of iatrogenic HAC and control of therapy), if necessary, imaging and biopsy. Trilostane is an effective drug against HAC. The starting dose of 1-2 mg/kg per day is effective for most patients, but it can be increased to 10 mg/kg in exceptional cases. In patients with iatrogenic HAC, the administration of glucocorticoids should be tapered gradually until discontinued.
Alopecia X
The pathogenesis of alopecia X has not yet been fully established. Predisposed breeds are Pomeranian, Chow Chow, Siberian Husky, Alaskan Malamute and Samoyed. Symmetrical non-inflammatory alopecia of the neck, caudal thighs and trunk are the dermatological lesions that occur without systemic clinical signs. The alopecia can appear both before and after castration. The diagnosis is made by excluding other diseases, especially endocrinopathies and performing a biopsy. There are various therapeutic options for alopecia X which include castration, melatonin, deslorelin, dermaroller and trilostane.
Follicular dysplasia
Follicular dysplasia causes non-inflammatory symmetric alopecia with hyperpigmentation in dogs. Seasonal flank alopecia (SFA), pattern baldness and follicular dysplasia of Doberman, Rottweiler, etc. are conditions included in this group.
SFA is the most common disease in the group. Hair loss begins in spring or fall and grows back after 3-6 months. Lack of melatonin could be the cause of hair loss. Among the predisposed breeds are boxers, bulldogs, Airedale terriers and schnauzers. The diagnosis is made based on the anamnesis and the exclusion of other diseases; a biopsy can confirm the diagnosis. Since melatonin (3-12 mg daily for approximately 2 months) stimulates hair growth, it can be administered to affected animals as prophylaxis at the beginning of the season.
Colour dilution alopecia (CDA) and black hair dysplasia
CDA occurs in dogs with a dilute coat colour. Black hair dysplasia occurs in dogs with a black coat or in areas of black hair. The hair is fragmented due to alterations in the formation of melanin. The observation of melanin clumps or macromelanosomes on the hair shaft by trichography is indicative of the condition. However, a definitive diagnosis can only be made by histopathological study. Melatonin therapy can be tried and existing secondary infections should be treated.
Telogen and anagen effluvium
Anagen effluvium is a follicular cycle disorder with acute interruption of the anagen phase, which can appear suddenly in serious illnesses or chemotherapy. Telogen effluvium developed more slowly over 1-2 months, and is assocated with malnutrition, stress, pregnancy or parturition. This condition is self-limiting, this is once the underlying cause is corrected, hair grows back in about three months.
An accurate history and clinical signs are of particular importance when working with inflammatory or non-inflammatory alopecia. Since the primary skin problem in non inflammatory alopecia can be complicated by secondary infections, cytology (by imprint or tape) should be used in all patients with alopecia to rule out secondary infections. Routine laboratory tests (blood chemistry, urinalysis) and specific tests should be performed, especially if endocrinopathies are suspected. In some cases, a biopsy is required to make a definitive diagnosis.
Dr Amir Davoodi, DVM. LABOKLIN – Department dermatology and allergy