Summer eczema is the most common itchy skin disease in horses. Synonyms are “insect bite hypersensitivity (IBH)”, “sweet itch”, “summer itch” or also “summer seasonal recurrent dermatitis (SSRD)”. On the one hand, pruritus is triggered by the sting of the insect itself and, on the other hand, by type 1 hypersensitivity to the salivary allergen of the insects.
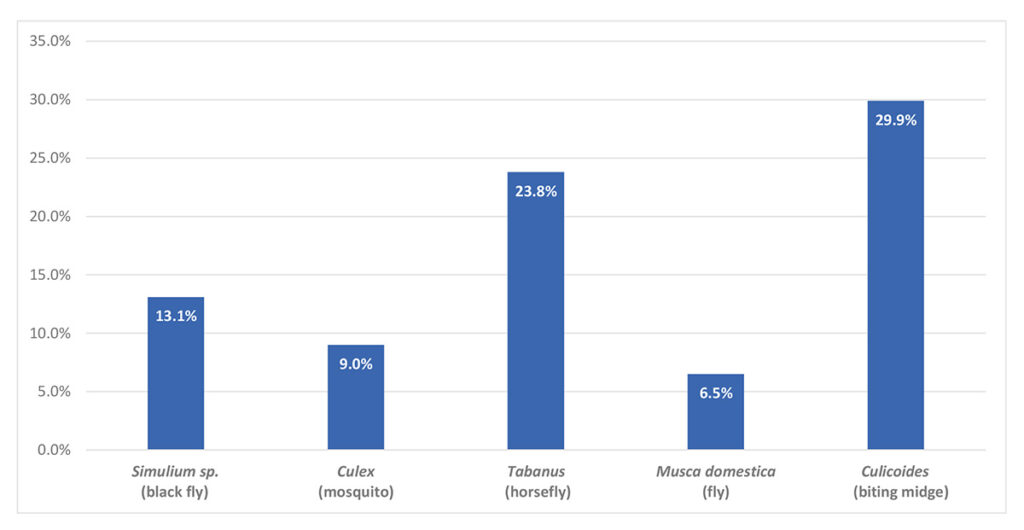
Apart from biting midges (Culicoides), other insects causing the disease are black flies (Simulium), flies (Stomoxys, Musca), mosquitoes (Culex) and horseflies (Tabanus). In one study, 75% of the horses reacted to Culicoides and to Simulium, which suggests a cross-reactivity. This is also supported by a study which showed that a homologous antigen can be detected in the salivary glands of both Simulium vittatum and Culicoides nubeculosus insects.
The tendency to develop insect bite hypersensitivity depends on various factors (e.g. genes, geographical location). Insect bite hypersensitivity is more likely to affect certain breeds, but the disease can occur in all breeds and at all ages.
The main reason why horses living in Iceland do not suffer from the disease is that Culicoides mosquitoes are not endemic to the country, which means that one of the main causes of the disease is missing. Animals born in Iceland and imported to Europe have an incidence of more than 50% (!) of contracting this allergy, whereas their offspring have an incidence of less than 10%. In another study, IBH occurred in 34.5% of 330 horses imported from Iceland to Denmark. Two years later, this figure had risen to 49.5% and to as much as 54% in areas with heavy mosquito infestation. Icelandic horses imported from Iceland to the USA did not show any symptoms in the first summer, but by the second summer, 56% were symptomatic. In contrast, only 4.6% of 1192 Icelandic horses born in German areas, where Culicoides mosquitoes are endemic, suffered from summer eczema. If both parents had IBH, prevalence increased to 12.2% and, in contrast, if only one parent had IBH, it decreased to 6.5%. However, if neither one of the parents was affected, prevalence was at 2.9%. Heritability with an incidence of 8.8% was also detected in Shetland ponies.
- Picture Credits: Dr Regina Wagner
- Fig. 1: Distribution pattern of sensitisation involving different insects
One author also found out that horses which had a proven history of summer eczema on the continent still exhibited significant sensitisation of their basophilic granulocytes to Culicoides after 15 asymptomatic years in Iceland. Even after such a long time, these animals had not lost their basic predisposition to develop summer eczema again when exposed to an appropriate allergen. In another study, Icelandic horses were imported from Iceland to Sweden. Horses which arrived in winter were twice as likely to develop IBH as those that arrived in summer. In Iceland, the animals have a high IgE titre due to worm infestation. Through endoparasite management after importation, it decreases, remains low in the healthy animal and increases again in animals suffering from eczema. When horses are imported in the summer, IgE against Culicoides competes with the antibodies produced due to the presence of endoparasites. During the winter IgE associated with endoparasites have decreased and there is no interference with IgE against Culicioides.
It was also found that IgE antibodies can be transferred from mother to foal via the colostrum. Both serum and cell-bound IgE could not be detected in unborn foals, but there was a clear peak 2 – 5 days after colostrum intake. These “maternal” antibodies are detectable in young animals during the first 4 months of life.
According to this study, endogenous IgE production begins at the earliest at an age of 9 – 11 months.
The first signs are usually seen at a young age (2 – 4 years). Generally, the clinical picture is strictly seasonal, highly pruritic and may be accompanied by papules or wheals.
All other efflorescences occur secondarily: alopecia, scales, crusts, excoriation, hyperpigmentation and lichenification. A dorsal and/or ventral distribution pattern is frequently seen. If the mane or the tail are affected, all that will typically remain is only a crusty hairless crest and a so-called “rattail”. Secondary bacterial infections of the damaged and traumatised skin are common and aggravate the itching even further.
The main differential diagnoses for insect bite hypersensitivity are atopic dermatitis (allergy to environmental allergens such as pollen, house dust and storage mites as well as moulds), food allergy, secondary bacterial infections and ectoparasites (biting lice/lice, Chorioptes and Psoroptes mites). Clearly, many animals do not only suffer from an allergic reaction to insects, but also to other allergens. An important indication in these cases is that the signs do not completely disappear in winter.
Diagnosis of insect bite hypersensitivity is based on the medical history (a single horse affected, seasonality) and the clinical picture (distribution pattern of pruritus and efflorescences). Skin scrapings should always be routinely examined to exclude the presence of ectoparasites. Cytology is also recommended for the diagnosis of secondary infections. In many cases, histopathology confirms the suspected diagnosis of an allergy, but does not provide any information on the type of allergen.
An allergy test can determine which insect species or which other seasonal allergens (e.g. pollen) are involved in the present disease.
Serological allergy tests offer a good opportunity to determine the causative allergen, but, as with other allergies, do not provide a diagnosis. The positive result is correlated with the medical history as well as the clinical picture and used to avoid allergens or to formulate ASIT (allergen-specific immunotherapy). Basically, it is necessary to distinguish between a skin allergy test (intradermal test), serological tests in which allergen-specific IgE are detected (ELISA), and cell stimulation tests. Very intensive research is carried out in order to establish allergy tests with recombinant allergens. In April 2021, for example, a study was published in which a microarray with Culicoides recombinant allergens was developed. There were 27 recombinant allergens of which 9 were major allergens for IBH with 7 of them being positive in more than 70% of IBH-affected horses.
Therapeutically, management is of great importance. Horses must be kept away from insects as much as possible. Various measures can be considered: keeping horses in a stable during the day and on the paddock at night, fine insect netting, fan in the stable, removal of standing water near the stable (old car tyres, cans …), eczema blankets, insect control with effective fly sprays (permethrin – caution: stable cats!, pyriproxyfen or icaridin).
Shampoo therapy or simply hosing down with cold water should also not be underestimated in order to reduce the percutaneous allergen load. Additionally, possible secondary bacterial infections are treated using an antibacterial agent (e.g. chlorhexidine 2 – 4%). The use of topical glucocorticoids is certainly justified in localised itchy areas. However, it is always important to bear in mind the withdrawal time (four weeks for topical preparations) in case an allergy test needs to be carried out!
Allergen-specific immunotherapy (ASIT, hyposensitisation) is the only treatment that provides causal intervention in the disease. It is used for insect bite hypersensitivity, urticaria caused by environmental allergens, atopic dermatitis, equine asthma or headshaking. In case of seasonal diseases, treatment should be started at the end of the season, i.e. in autumn for animals suffering from summer eczema. Therapy must be carried out for at least 12 months in order to be able to accurately determine its efficiency. If it is successful, it should be carried out for the rest of the horse’s life. The allergens included must correlate with the medical history and the clinical picture and should be selected specifically for the patient. The success rate of ASIT ranges from 60% to 70%. If the test result is positive (intradermal or blood allergy test) and correlates with the medical history and the clinical picture, this form of therapy is a treatment option which is rarely accompanied by side effects and which is cost-effective (weight-independent costs (!)). After the initial treatment phase, only occasional applications are required in the further course of the disease and this implies, in addition to cost efficiency, less effort for the owner (the maintenance dose is usually a subcutaneous injection every 4 weeks). This type of treatment can also be carried out on sport horses, as these animals often return to a good performance level and yet are not treated in a doping-relevant way.
New promising treatments, such as an active vaccine against IL-5 or IL-31, have been published but are not yet ready for the market.
In summary, it should be noted once again that allergies are very common in horses, the disease is not curable, but various diagnostic and therapeutic options allow for good management of the disease as long as the owner is properly informed and willing to cooperate.
Dr. Regina Wagner
The book “Allergene bei Tieren” can be ordered here: