The pancreas is a very important digestive organ in dogs and cats and consists of an exocrine and endocrine portion. The exocrine pancreas is a serous gland that secretes enzymes that are essential for the digestion of all relevant types of nutrients. Anatomically, it is made up of the acini and the duct system. The enzymes are produced by the secretory cells in the acini and are stored in granules.
1. Pancreatitis
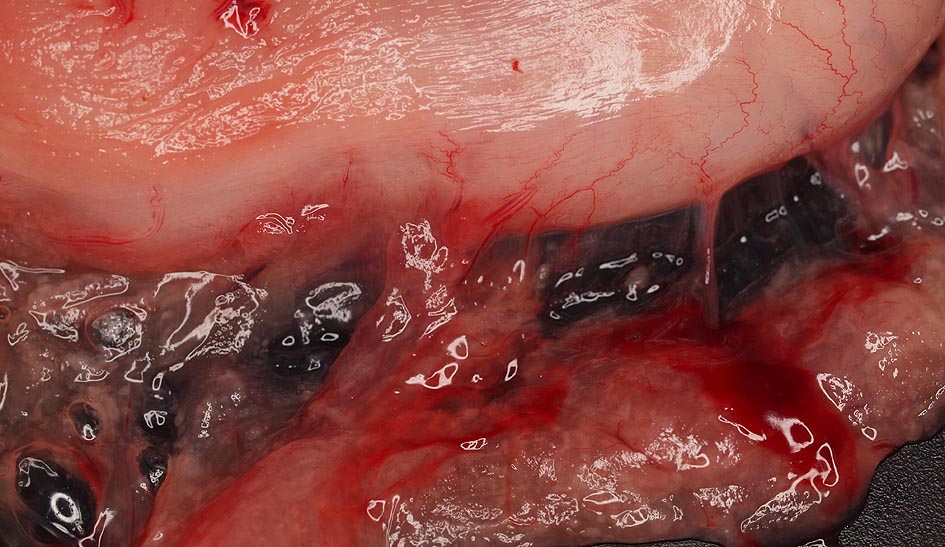
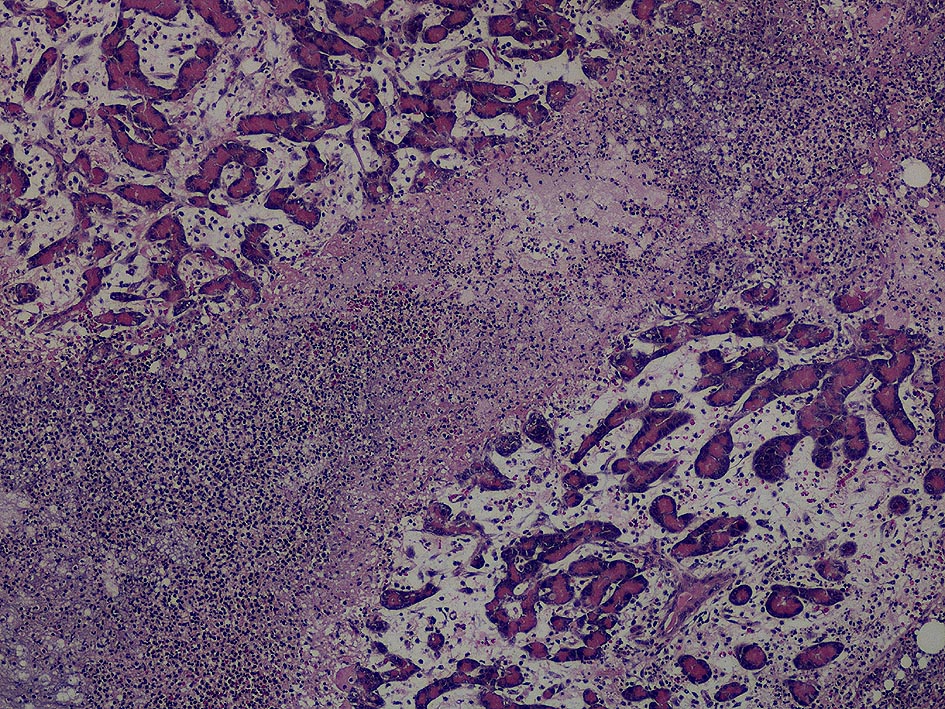
A pancreatitis is a very painful inflammation of the pancreas, caused by early activation and release of proteolytic enzymes from the acinar cells. The result is local and systemic destruction of tissues by the pancreatic enzymes themselves and by inflammatory mediators that are released during this process. Middle aged dogs and cats are most commonly affected. Miniature Schnauzers, Yorkshire Terriers, and Poodles are prone to pancreatitides. Siamese cats appear to be more commonly affected than other cat breeds. (Fig. 1 + Fig. 2)
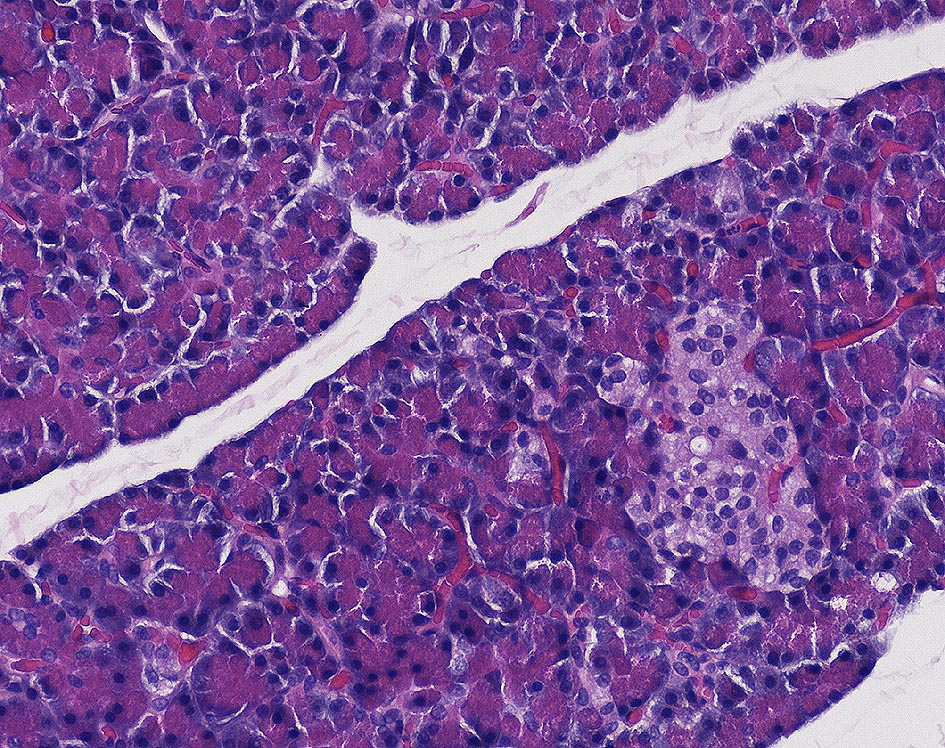
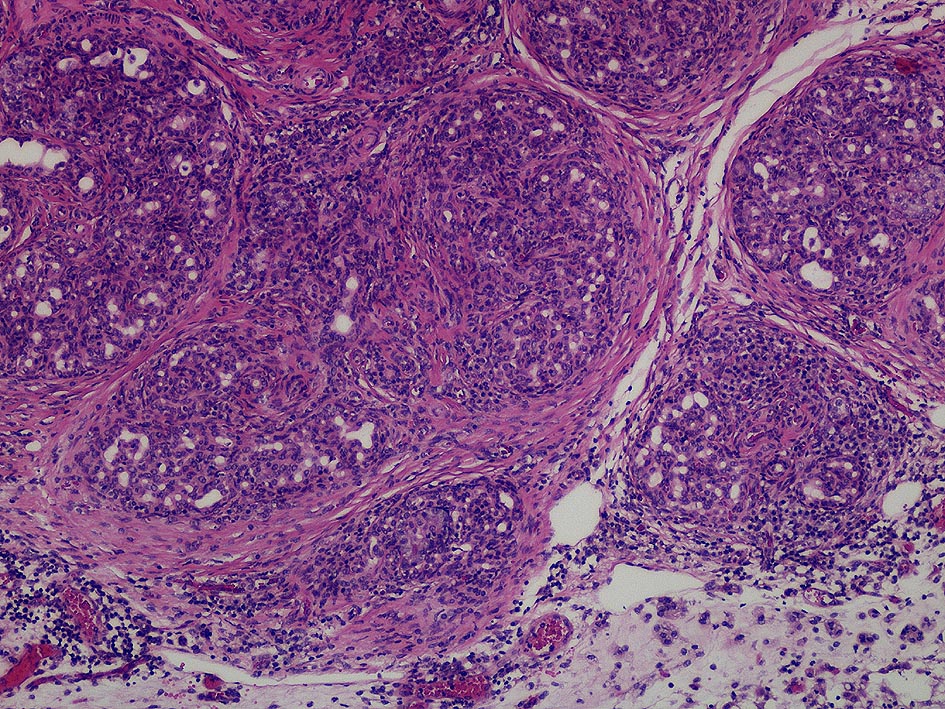
Pancreatitis has long been known as a disease in companion animals. Inflammatory changes were first noted more or less accidentally during dog and cat necropsies. This led to the hypothesis that pancreatitides are much more common in dogs and cats than previously supposed. Numerous researchers have since contributed to a better understanding of this disease. However, although we now know that diseases of the exocrine pancreas, especially pancreatitis, are much more common in dogs and cats than originally supposed, clinical diagnosis and treatment have not become easier. The principal signs of disease are very unspecific and include anorexia, vomitus, abdominal pain, weakness, diarrhoea, (icterus in cats). Not all signs are present in all cases and in very mild cases no clinical signs may be detected. In cats, the signs are even less clear than in dogs. For this reason, pancreatitis should always be included in the list of differential diagnoses in cases of gastrointestinal disease. (Fig. 3 + Fig. 4)
2. Pancreatitis – Diagnosis/Laboratory Diagnosis
Blood count and clinical chemistries usually only show unspecific changes that may be related to vomiting and diarrhoea. The changes do not help in reaching a diagnosis, but can help evaluate the health status of the patient.
2.1. Amylase/Lipase
These are not pancreas specific enzymes and are also found in the intestine, the muscles, the salivary glands, and the liver. The sensitivity of lipase is about 55% in dogs. A 3-fold lipase increase is relatively specific in dogs, but lipase is not always elevated in cases of pancreatitis. In cats, lipase is even less specific than in dogs. Both enzymes may be increased in liver and kidney disease, in cases with neoplasia or following treatment with glucocorticoids and diabetic ketoacidosis.
2.2. TLI (Trypsin-like Immunoreactivity)
This assay measures trypsin and its precursor trypsinogen. Trypsinogen is synthesized exclusively in the pancreas. However, only 30-60% of the dogs and cats with pancreatitis have measurable increases in this value. This is probably due to the very short half-life of the enzyme. Feeding and kidney disease also lead to increased values. The TLI is a better diagnostic marker for exocrine pancreas insufficiencies.
2.3. PLI (Pancreatic Lipase Immunoreactivity)
Pancreas lipase is synthesized exclusively in the acinar cells of the pancreas. Physiologically, only small amounts of pancreatic lipase are found in the peripheral circulation. If acinar cells are destroyed during the course of a pancreatitis, increased amounts are released into the circulation. The degree of increase correlates with the degree of inflammation and destruction of the pancreas. The pancreatic immunoreactivity is determined by structural characteristics specific for pancreatic lipase. This is a significant difference from other assays which determine the lipase activity. The activity, however, is identical for all lipases, independent of the tissue from which they originated. Specific tests for the quantification of feline (fPLI) and canine (cPLI) pancreatic lipase have been developed. The specificity is around 71% in dogs with a sensitivity of 93%. In cats, the assay is 91% specific and 67% sensitive. The determination of PLI is not influenced by enzyme substitution and neither haemolysis nor lipaemia affect the determination. PLI is very stable. The determination of PLI in serum from dogs and cats is currently considered the most reliable non-invasive test for the diagnosis of pancreatitis.
-
Fig. 1: Acute, purulent pancreatitis in a 12 year old cat that died peracutely
source: Aupperle, Laboklin
-
Fig. 2: Acute, purulent pancreatitis in a 12 year old cat that died peracutely
source: Aupperle, Laboklin
-
Fig. 3: Healthy pancreatic tissue, cat
source: Aupperle, Laboklin
-
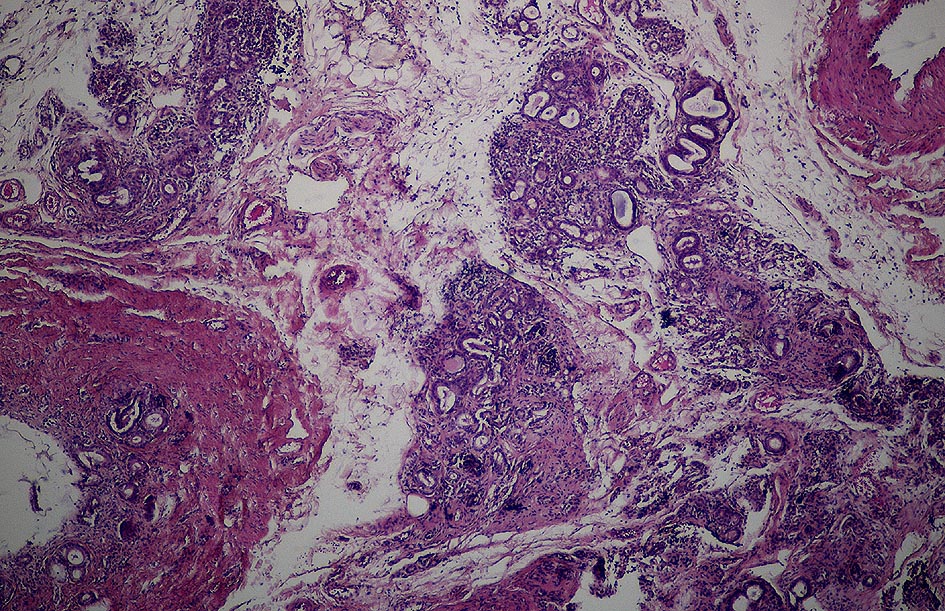
Fig. 4: Chronic pancreatitis with increasing tissue fibrosis
source: Aupperle, Laboklin
-
Fig. 5: Pancreatic atrophy, final stage, in a dog. The severely reduced glandular tissue (stained blue) is clearly visible
source: Aupperle, Laboklin
3. Exocrine Pancreatic Insufficiency (EPI)
In cases of EPI, the synthesis and secretion of pancreatic enzymes are insufficient, leading to maldigestion and malabsorption. Clinical signs occur when the functional tissue has been reduced to 10-15%. An EPI can manifest itself in weight loss despite normal or increased appetite. Affected animals often suffer from chronic diarrhoea and the coat may appear shaggy and dull. The faeces of affected dogs is often unformed, very voluminous and may be yellowish and fatty and contain undigested food. An EPI can be congenital or acquired. German Shepherds and Collies can have a genetic defect that causes pancreatic acinar atrophy (PAA). Affected dogs develop clinical signs at a very young age and can become severely cachectic. EPI is very often a result of chronic recurring pacreatitides that have not been recognized and treated. In these cases it is a disease of middle aged or old dogs and cats. In rare cases, pancreatic neoplasia can lead to EPI. If the EPI is a consequence of a chronic recurring pancreatitis, diabetes mellitus can develop as a secondary complication. In almost all cases, EPI is associated with vitamin B12 deficiency. This is due to the fact that intrinsic factor, which is necessary for the resorption of vitamin B12 in the ileum, is synthesized in the pancreas. Necessary buffer systems and antimicrobial substances, which are also products of the exocrine pancreas, are also lacking. Inflammatory bowel disease (IBD) therefore often develops during the course of EPI. In cats, EPI is rare and is usually the result of a chronic pancreatitis or an obstruction of glandular discharge (adenocarcinoma). (Fig. 5)
4. EPI Diagnosis
4.1. Clinical Chemistry and Blood Count
Often unremarkable.
4.2. TLI (Trypsin-like Immunoreactivity)
As mentioned above for pancreatitis, TLI determines trypsin and its inactive precursor trypsinogen in the serum of dogs and cats in species specific assays. It is the test of choice for the diagnosis of exocrine pancreatic insufficiency. The sensitivity and specificity of TLI are near 100% in dogs. The sensitivity in cats is unknown, but the specificity is between 85 and 100%. EPI is characterized by a decreased TLI serum concentration, although a single low TLI value without corresponding clinical signs is not diagnostic of EPI and should be confirmed after a few weeks. Only if the serum TLI concentration is persistently reduced is there proof of an EPI.
Careful: the animal must fast (8, better 12 hours) before sampling. Food intake leads to artificially increased values. False high values are also found in conjunction with kidney insufficiency and in severely cachectic dogs.
4.3. Pancreatic Elastase
Pancreatic elastase is an endoprotease that is resistant to digestion which is exclusively synthesized in the acinar cells of the pancreas. It can currently only be measured in faecal material from dogs. There is no corresponding assay available for cats. Pancreatic elastase levels are significantly reduced in exocrine pancreatic insufficiencies, but can also be reduced in healthy dogs, so that a positive result should be confirmed by a follow-up determination of TLI (specificity 50%). It should be noted that there is a “dilution effect” in patients with diarrhoea. In these cases, the test should be repeated and the serum TLI should be determined.
4.4. Vitamin B12 (Cobalamin)/Folic Acid
These are both water soluble vitamins of the B-complex. They cannot be synthesized by the body and must be ingested from the diet. Commercial foods general contain sufficient amounts of both vitamins, making food based deficiencies improbable unless an animal is fed an exclusively vegetarian diet. Vitamin B12 is bound to food proteins and must be cleaved from these with the help of pancreatic enzymes, and then bound to intrinsic factor, which is also synthesized in the pancreas, in order to be resorbed in the ileum.
In cases of exocrine pancreatic insufficiency, insufficient intrinsic factor is synthesized, reducing the resorption of vitamin B12 in the ileum. Many intestinal bacteria also digest vitamin B12, which increases the deficiency. Folic acid is absorbed via specific receptors in the small intestine. Damage of those receptors during the course of a disease can lead to a deficiency. A folic acid surplus can also occur in cases of overgrowth or miscolonisation of the small intestine, since intestinal bacteria are able to synthesize folic acid. Since EPI often leads to shifts in the intestinal flora, changes in folic acid and vitamin B12 concentration can be helpful for diagnostics. These interdependencies demonstrate that an EPI can easily cause vitamin B12 deficiency and increased serum folic acid levels. Checking both vitamins is therefore recommended for all patients with gastrointestinal signs and/or suspected EPI.