Clinical history
Hass, an 18-month-old male, mixed-breed dog weighing 42 kg, was presented with a six-month history of a rash on his legs and ears. The condition did not bother him but was not improving. The animal was happy and active. He had been treated with corticosteroids showing slight improvement during the treatments. He was off from medication for a month, and the condition was spreading. A fortnight ago, he received an injection of Ivermectin. He lived in a house with a garden with two other dogs without lesions and had no ectoparasite protection (Fig. 1).
Dermatological examination
Dermatological examination showed an extensive papular reaction with marked erythema of all extremities, more intense on distal areas to the elbow and inter-pad and inter-digital areas. There was partial June 2020 alopecia and foci of exudation with scabs. The extremities were slightly edematous. On the abdomen and in the pinna, there was a diffuse erythematous micro-papular rash.
There was no pruritus or pain associated to the affected areas, no pruritic reflex when rubbing the lesions or the trunk (negative truncal pedal reflex).
The popliteal lymph nodes were slightly enlarged, but there was no notable lymphadenopathy (Fig. 2).
Dermatological pattern
The dermatological pattern was defined as: severe erythematous papular dermatitis affecting the extremities, abdomen and pinna, with alopecia in extremities and no pruritus.
Differential diagnoses
The suggested differential diagnoses were: erythema multiforme, contact dermatitis, Leishmaniosis, Borreliosis, Ehrlichiosis, Filariasis, lymphedema, eosinophilic mucinotic mural folliculitis, demodicosis or bacterial folliculitis.
Diagnostic tests
Trichography revealed no parasites, no fungal elements and no lesions compatible with fungal infection. The anagen/telogen index was 1/1.
No bacteria or Malassezia sp. were found on superficial skin cytology.
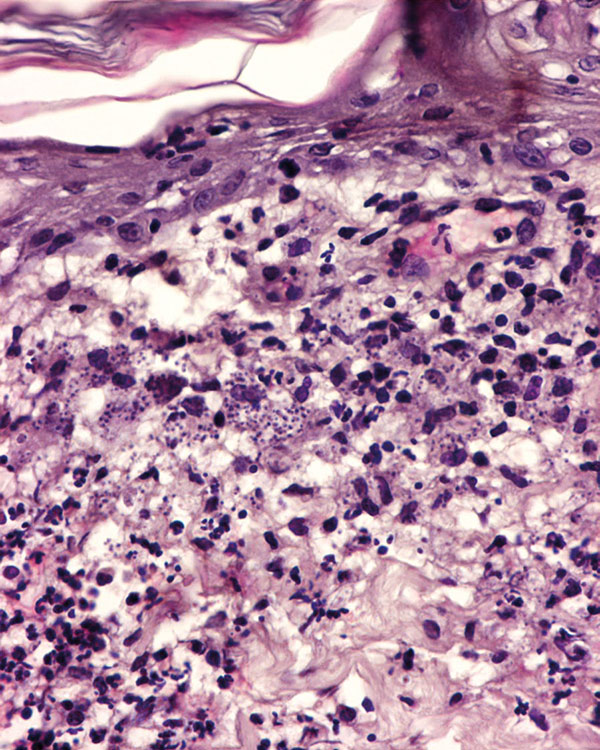
Four 8 mm skin punch biopsies were obtained. The histopathological study revealed a mononuclear dermatitis from nodular to diffuse with the presence of Leishmania amastigotes inside macrophages (Fig. 3).
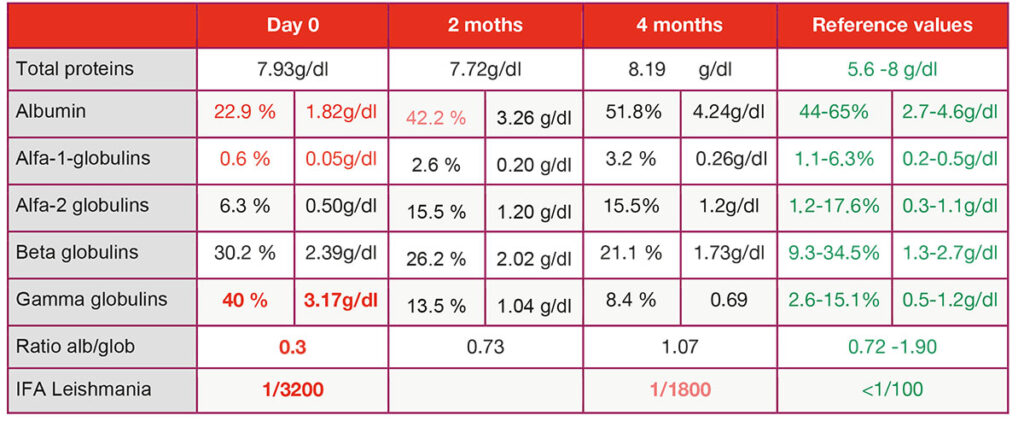
A complete leishmania profile showed normal haematological and biochemical values, except for alterations in protein electrophoresis with hypoalbuminaemia and hyperglobulinaemia. The A/G ratio was 0.30 (Table 1). The antibody titer against Leishmania by IFA was 1/3200.
A rapid test for Borrelia sp., Ehrlichia sp., Filaria sp. and Anaplasma sp. was negative.
Diagnosis
Leishmaniose
Treatment
Treatment was started with 600 mg Allopurinol every 12 h and Glucantime® (Meglumine Antimoniate) SC – 14ml every 24h for four weeks (Fig. 4).
Outcome
At the end of the Glucantime® treatment (day 28), all the lesions had resolved. After 60 days of treatment, protein electrophoresis showed normalisation of all values. The therapy with Allopurinol was maintained for four months, at that time, the proteinogram was in range, and the leishmania antibody titer was reduced to half. Subsequent controls were maintained in normal range, and the animal has not suffered any subsequent relapse, the antibody titer being negative.
Discussion
Leishmaniosis is a zoonotic disease, endemic in Mediterranean countries. Leishmania infantum is responsible for practically all cases of Leishmaniosis in Europe. Phlebotomus sp. is the insect vector, which inoculates the flagellated promastigotes, the infective form of the parasite. Once in the skin, the promastigotes lose the flagella and transformed into amastigotes.
- Fig. 1: Picture Credits: Dr. Carmen Lorente
- Fig. 2: Picture Credits: Dr. Carmen Lorente
- Fig. 3: Picture Credits: Dr. Carmen Lorente
- Fig. 4: Picture Credits: Dr. Carmen Lorente
- Tab. 1: Result of protein electrophoresis
- Fig. 5: Histological picture of the lesions in this case: mononuclear inflammatory infiltrate with a large number of leishmania amastigotes inside macrophages
The development of the disease depends on the individual’s immune response. A cellular or Th1 response would be protective controlling the parasite at the entry point, while excessive antibody production in the absence of a cellular response would induce disease development.
Hass presented an unusual form of leishmaniosis with a papular cutaneous process in the absence of systemic signs of disease. Presence of leishmania amastigotes in skin biopsy diagnosed the infection, indicating the direct participation of the parasite in the inflammatory reaction causing the dermatological condition. The systemic involvement must always be assessed by complementary blood tests: haematology, blood biochemistry, leishmania serology and protein electrophoresis.
Papular dermatitis has been described as a benign cutaneous condition of leishmaniosis in animals with a good cell-type response. It is usually associated with low antibody titer, absence of alterations in protein electrophoresis and proper response to treatment. Probably, in this case, the late diagnosis of the process and the successive treatments with glucocorticoids favoured the dissemination of the parasite and a deviation to a humoral type immune response with antibody production and electrophoresis alteration. However, at the time of diagnosis, no general clinical signs of disease were detected.
It is essential to define the clinical stage of the disease to give a prognosis and establish the most appropriate treatment. Four clinical stages are described: mild, moderate, severe and very severe, depending on the clinical picture and the clinicopathological findings. In this case, the disease was classified as stage II, or moderate, based on the presence of skin lesions, clinicopathological alterations (hypoalbuminaemia and hyperglobulinaemia) and a high titer of anti-Leishmania antibodies.
The treatment was adapted to the indications of the Leishvet Guide and the ESCAPP which establishes the use of Allopurinol (10 mg/kg every 12 h PO) + Glucantime® (100 mg/kg every 24 h for 4 weeks).
The response to treatment was excellent with complete resolution of the lesions and normalisation of the proteinogram. Four years later the dog is still healthy and the leishmania titer converse is negative (Fig. 5).
Dr Carmen Lorente Méndez, DVM, PhD, DipECVD. EBVS® European Specialist in Veterinary Dermatology