As the liver plays a major role in an array of metabolic processes, liver diseases are connected with various clinical findings and clinicopathologic abnormalities.
Clinical signs
Early clinical signs are usually unspecific such as intermittent appetite, weight loss, polyuria/ polydipsia, occasional vomiting or diarrhea and lethargy. As the liver has an enormous reserve capacity, more specific signs as icterus, hepatic encephalopathy, bleeding tendency or ascites develop late in the disease progress. These findings are the consequence of a decreased liver function.
Laboratory evaluation
Clinicopathologic changes in the course of liver diseases are as variable and non-specific as the physical findings, nevertheless liver disease is often first diagnosed during routine blood tests.
It is particularly important to distinguish between enzyme diagnostics and liver function tests.
Increased activities of „liver enzymes“ are either due to liver cell damage (ALT, AST, GLDH) or enzyme induction (AP, GGT) caused by cholestasis or by drugs. There are also a number of extrahepatic conditions that cause increases in enzyme activities. However, enzyme elevations don’t provide any information on the degree of liver damage or liver function.
To evaluate the function of the liver, concentrations of substances are measured, which are synthesized or metabolised in the liver, and/or excreted by the liver/bile (bilirubin, bile acids, albumin, coagulation factors, urea, glucose).
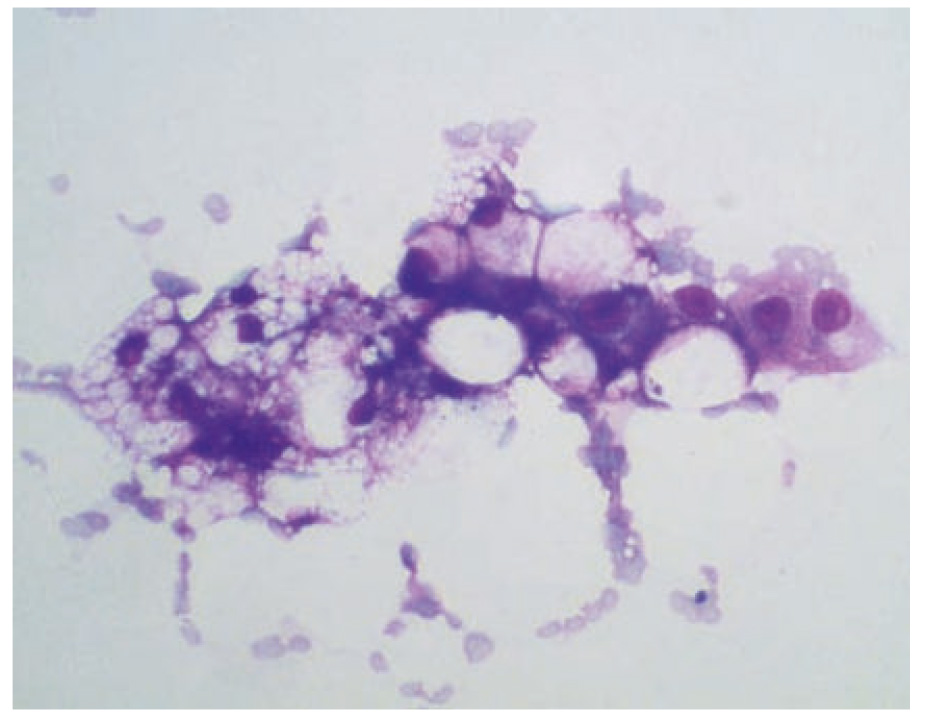
- Fig. 1: Cytologic appearance of hepatic lipidosis
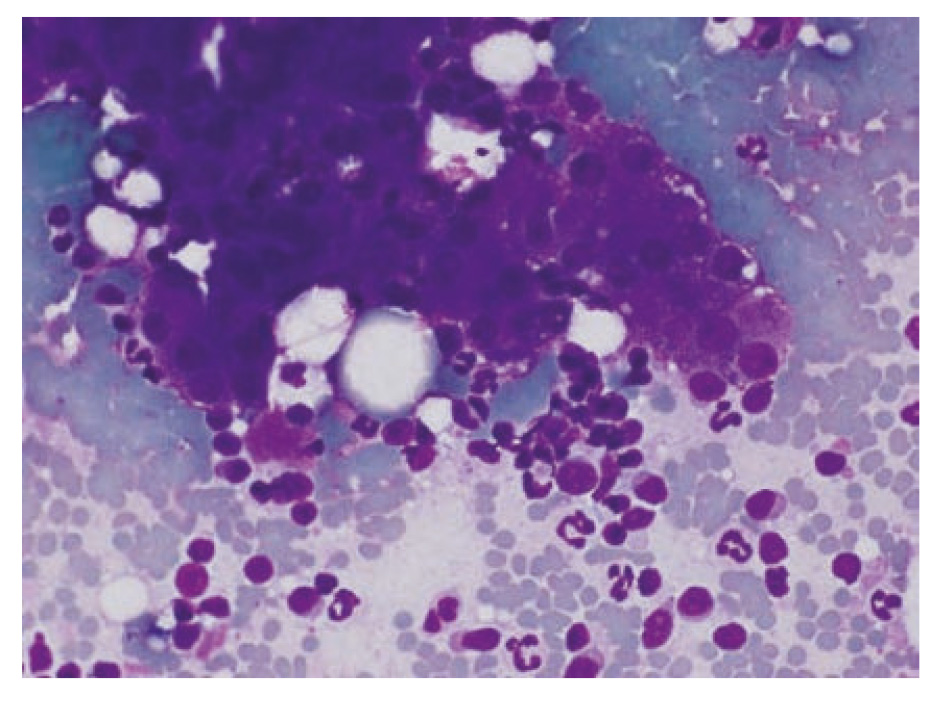
- Fig. 2: FNAB: Cluster of hepatocytes surrounded by neutrophils and lymphocytes
Enzymology in the cat
ALT (alanine amino transferase) is a liver-specific enzyme. An increase in activity can occur in any type of liver injury, as well as in the course of extrahepatic processes. Following acute liver injury, activity can increase to a 100-fold within a few hours. When the damaging insult stops, ALT activity decreases to within the reference interval within 1 to 3 weeks.
AST (aspartate amino transferase) is less liver-specific than ALT, as activity is also high in the skeletal muscle and erythrocytes. Hence the serum activity is increased in liver cell damage, muscle damage, or haemolysis.
After an acute insult AST rises more slowly and to a lesser extent than ALT. Because the halflife of AST is shorter (77 minutes in the cat) its activity decreases to the reference range faster after cessation of the insult than ALT. Persistent elevation of AST serum activity indicates a poor prognosis.
GLDH (glutamate dehydrogenase) is present in the mitochondria of hepatic cells, which are present in the perivenous liver cells in a particularly large number. These perivenous areas of the liver lobule are the first to be damaged by hypoxic and metabolic insults, as well as cholestatic processes. A selective increase in GLDH activity may therefore indicate congestion.
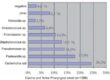
| Extrahepatic causes of liver enzyme elevations |
|
Increased activity of feline AP (alkaline phosphatase) should be interpreted differently than in dogs. Cats have less hepatocellular AP, which also has a very short half-life. Therefore, any increase in enzyme activity in the blood is important and should be investigated. In addition to increases due to extrahepatic conditions, AP activity in cats is especially elevated in hepatic lipidosis and cholangitis. In hepatic lipidosis cats usually show a considerably greater increase of the AP compared to the increase of GGT.
GGT (γ-glutamyl transferase) is a membranebound enzyme like AP and present in many tissues. The highest activities are found in the kidney and pancreas, however, since renal GGT is excreted in the urine and pancreatic GGT is secreted into the duodenum, the majority of serum GGT activity derives from the liver, with the exception of the increase in puppies after ingestion of colostrum. In the cat GGT is a sensitive parameter for the diagnosis of cholestasis.
Functional diagnostics
Albumin is synthesized in the liver, but its serum concentration is subject to many extrahepatic influences and therefore relatively unspecific for liver disease. Extrahepatic causes of hypoalbuminemia which should be excluded, include protein losing enteropathy, proteinuria, exudative skin lesions, malnutrition and sequestration into third compartments (eg ascites).
The major part of the coagulation factors are synthesized in the liver. Severe acute and chronic liver diseases can lead to coagulation disorders. Prothrombin time and activated partial thromboplastin time may be prolonged, which requires particular importance when the performance of a liver biopsy is planned.
Urea is synthesized in the liver via the urea cycle from toxic ammonia. Severe hepatic disease and portosystemic shunts can result in decreased levels of urea, with a corresponding increase in the plasma ammonia concentration.
The liver has a large reserve capacity to maintain glucose homeostasis. Nevertheless, hypoglycaemia may occur in the final stage of chronic hepatitis, liver failure and portosystemic shunts.
Bilirubin serum concentration provides information on its uptake by the liver cell, the conjugation and excretion into bile. However, this analyte is not very liver-specific, since there are also extrahepatic causes for increased bilirubin levels, such as hemolytic anemia and extrahepatic cholestasis. The different forms of hyperbilirubinemia can be distinguished by joint interpretation of other laboratory findings or results of diagnostic imaging. For each jaundiced patient a hematologic examination should be performed in order to exclude hemolysis.
Bile acids are synthesized in the mitochondria of hepatocytes from cholesterol and then conjugated mainly with taurine. Because of the conjugation the primary bile acids are present in ionized form in the intestines and can not be reabsorbed initially. Only after the emulsification of dietary fat are bile acids reabsorbed by specific receptors in the ileum and transported back to the liver via the portal vein. The majority of bile is stored in the gallbladder, about 10-20% of bile acids are secreted into the duodenum continuously and represent the so-called fasting bile acids. In healthy animals, the serum concentration of bile acids (postprandial) increases mildly after food intake due to the gallbladder contraction, the bile acids are reabsorbed from the intestine and transported back to the liver in the portal blood (enterohepatic circulation). The large amount of bile acids exceeds the clearance capacity of the liver cells. The most relevant information is obtained by paired measurement of both the pre-prandial (after 12 hours of fasting) and postprandial (2 hours after a test meal) bile acid concentration, although the specificity of the individual measurements is very high.
Increased bile acid concentrations indicate a dysfunction of the liver (or abnormalities of the liver vessels), even before the onset of jaundice.
Haematology
Anaemia is a frequent finding in the course of liver disease, which in the case of bleeding (coagulopathy, gastrointestinal ulcers) is regenerative. More commonly, however, aregenerative anaemia is present due to inefficient utilization of iron stores.
Inflammatory liver diseases can be accompanied by leukocytosis.
Urinalysis
The specific gravity may be lowered due to polyuria / polydipsia frequently occurring in the course of liver disease.
In the urine of healthy cats bilirubin is not detectable, hence any bilirubinuria is a significant finding and necessitates further diagnostic wor-kup.
15% of cats with portosystemic shunts and cats suffering from severe liver dysfunction show ammonium biurate crystalluria.
Biopsy
The clinical examination, laboratory and diagnostic imaging procedures can only provide the organ diagnosis „hepatopathy.“ The definitive diagnosis of the underlying disease process can
only be determined by the examination of biopsy samples.
There are different methods available to obtain a tissue sample. The simplest techniques are the fine needle aspiration (FNA) and core biopsy.
They can be performed blind or ultrasound-guided, punch biopsies are also performed laparoscopically.
Cytological examination of FNAs has many advantages, such as the minimum cost of materials and the rare occurrence of complications during the sampling procedure. However, studies show that the diagnosis of cytology and histopathology show a complete agreement in only 30% of the cases.
Common feline hepatobiliary disorders
Hepatic lipidosis
Feline hepatic lipidosis is a common and potentially lethal disease. Obese cats show a predisposition to the development of hepatic lipidosis. In 5% of all cases, the lipidosis is idiopathic, but mostly there is an underlying condition or disease that causes a catabolic state. The influx of fatty acids from body fat stores exceeds the capacity of the liver to process them. (Fig. 1)
Commonly, middle-aged, obese cats are affected. They show a history of inappetence for some days, weight loss, lethargy and sometimes vomitus. The margins of the enlarged liver are palpable and 70% of the patients are icteric.
Laboratory abnormalities can be varied depending on the existence of underlying diseases. Typically there is a marked increase in AP activity accompanied by only moderate increases of the activity of ALT and AST. A concurrent marked increase in GGT activity indicates an underlying pancreopathy or cholestatic hepatopathy. Hyperbilirubinaemia and markedly increased bile acid concentrations are common.
| Treatment of hepatic lipidosis |
|
Neutrophilic cholangitis
Neutrophilic cholangitis occurs predominantly in middle-aged to old cats. The onset of disease is mostly acute and patients show anorexia, lethargy and fever. Most animals are jaundiced and palpation of the cranial abdomen is painful. Cases of chronic neutrophilic cholangitis are associated with mild symptoms.
Characteristic laboratory abnormalities are hyperbilirubinaemia and increases in ALT and to a lesser extent AP and GGT activity. Bile acid concentration is usually increased.
Haematological examination shows leukocytosis with neutrophilia, frequently with a left shift. Cultural examination of liver tissue or bile is recommended, as neutrophilic cholangitis is believed to result from ascending bacterial infection from the intestine.
Neutrophilic cholangitis is frequently associated with pancreatitis and IBD (inflammatory bowel disease).The presence of all three conditions simultaneously is called triaditis. Most likely the IBD predisposes to ascending bacterial infections in the liver and pancreas.
| Treatment of neutrophilic cholangitis |
|
Lymphocytic cholangitis
Lymphocytic cholangitis occurs in young cats, about 50% of the affected animals are under the age of 4 years. Persians are predisposed.
The aetiology of lymphocytic cholangitis is unclear, it is assumed to be an immunemediated process.
The clinical presentation is very mild in the beginning, the appetite is maintained or even enhanced while the animals lose weight. The main symptoms are jaundice and ascites, although these findings frequently are not very pronounced initially. Hepatomegaly and lymphadenopathy may occur.
In mild cases or early stages the only laboratory abnormalities are mild increases in the activity of all liver enzymes. In more advanced cases, bilirubin and bile acid concentrations are markedly increased. Most often the total protein concentration is increased due to hypergammaglobulinemia. FIP is an important differential diagnosis of lymphocytic cholangitis, as the characteristics of the ascites occurring in both diseases is very similar.
| Treatment of lymphocytic cholangitis |
|
Mixed inflammatory cholangitis
There are some cats showing a mixed inflammatory infiltrate In these cases it is very difficult or impossible to determine whether the primary inflammatory process was neutrophilic or lymphocytic. The clinical signs are mild and nonspecific: varying appetite, weight loss and lethargy are dominant. Sometimes an acute onset of the disease can be determined, which then suggests a case of neutrophilic cholangitis that has become chronic.
Mixed inflammatory cholangitis represents a therapeutic challenge because the treatment of neutrophilic and lymphocytic cholangitis is contradictory. While antibiotic treatment is the priority in the former, with the latter glucocorticoid therapy is essential. In mixed inflammatory cholangitis it is therefore recommended to initiate antibiotic therapy first and, if there is no significant improvement within 1-2 weeks, administer prednisolone at anti-inflammatory doses, additionally. (Fig. 2)