When to suspect hemolysis?
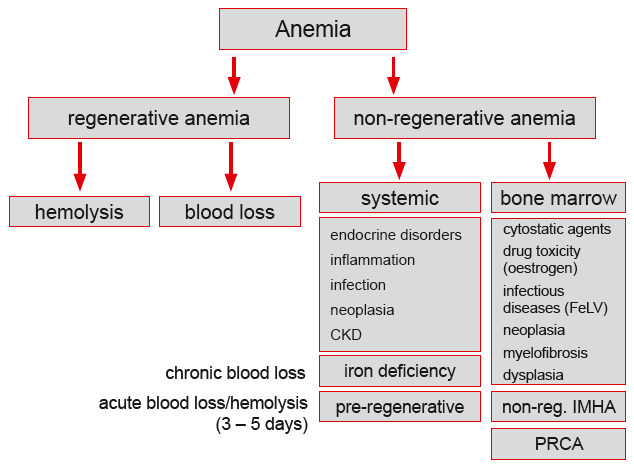
We suspect hemolysis especially in regenerative anemia when blood loss has been excluded (Fig. 1).
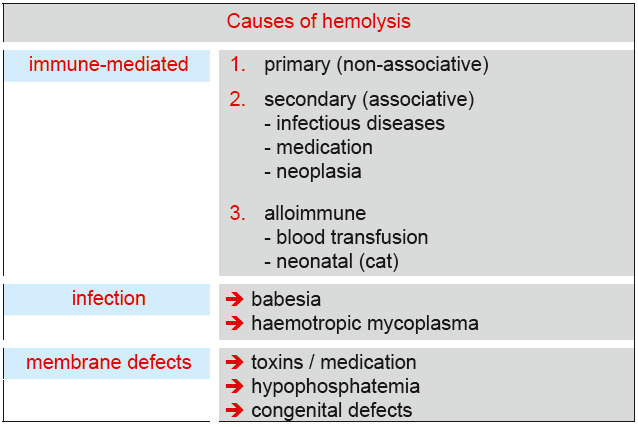
In most cases, hemolytic anemia are severe and show stronger signs of regeneration than blood loss anemia. In case of hemolysis, erythrocytes are destroyed. In addition to primary IMHA (referred to as non-associative IMHA), a variety of underlying diseases can cause hemolysis (Fig. 2).
Which tests should be performed?
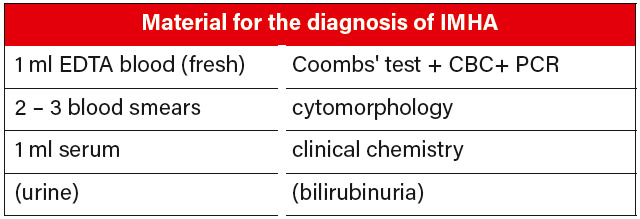
Requested material for the diagnosis of IMHA are listed in Fig. 3.
CBC/cytomorphology (blood smear):
Provides information regarding regeneration and is useful as a first overview, e.g. to detect infectious agents. Erythrocyte morphology can also provide important information regarding the cause of anemia. At Laboklin, a reticulocyte count is included in every canine and feline CBC. The CBC should be measured from EDTA blood as soon as possible after blood collection as the erythrocyte fragility of dogs with IMHA is increased.
Blood chemistry: Measurement of serum bilirubin and total protein to identify the cause of anemia can help to differentiate between hemolysis and hemorrhages.
Urinalysis: In some cases of hemolysis, bilirubinuria or hemoglobinuria may be present. Please note that in dogs – especially in male dogs – a weakly positive test result can be physiological.
Infectious agents to detect infectious agents such as babesia and haemotropic mycoplasma in acute phases, molecular analysis (PCR) is recommended. Additionally, pathogens such as ehrlichia and anaplasma should be excluded. For ehrlichia, an additional antibody titer determination is useful.
Tests to diagnose immune-mediated destruction
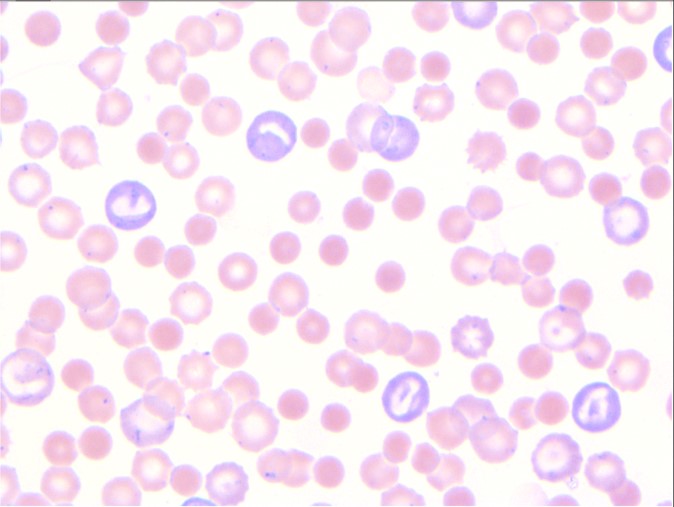
Spherocytes: The presence of so-called spherocytes (Fig. 4) in the blood smear can provide valuable information about an immunemediated destruction of the erythrocytes. The sample material required for their detection are two to three blood smears directly made in the practice.
Autoagglutination: By looking at the EDTA sample, one may notice the presence of an unspecific autoagglutination. This finding should be followed by a saline agglutination test and a Coombs’ test.
Coombs’ test: Suitable to detect the presence of autoantibodies on the surface of erythrocytes. Sample material: Fresh EDTA blood. If the sample is kept refrigerated, the test can be evaluated up to 5 days from collection.
FAQs on assessing the Coombs’ test
What is the principle of the Coombs’ test?
The Coombs’ test, also named DAT (Direct Antiglobulin Test), is testing for the presence of antibodies on the surface of the red blood cells (Fig. 5).
Different test methods are available on the market: gel test, strip test, flow cytometry test, the well-known microtiter plate test, and more. All the mentioned tests are adequate for the diagnosis of IMHA in humans and dogs. Some tests are also available on the market for cats and horses.
What is the principle of the microtiter plate method?
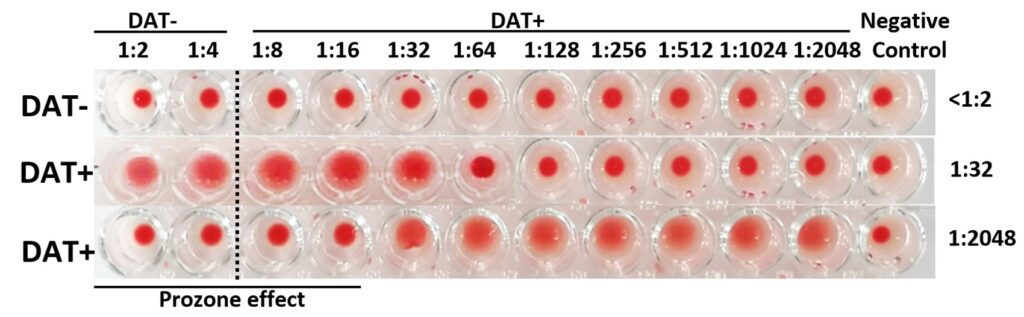
In veterinary medicine, the microtiter plate is the most commonly used method. The antiglobulin (Coombs’ reagent) is gradually diluted (1:2, 1:4, 1:8, 1:16, etc.), then washed erythrocytes are added and incubated for at least 30 minutes. If no reaction occurs, the blood cells will sediment at the bottom of the wells and only a tiny red point will be observed after incubation: the test result for this well is negative. If the test is positive, the added antiglobulins bind the erythrocytes, refraining them from falling to the bottom of the well. The erythrocytes cover the well completely, or almost completely. If only the two first wells (1:2 and 1:4) show positivity, the test is still considered negative, because these low titers are considerated unspecific. Titers from 1:8 are considerate positive. It is not rare to see titers above 1:1024 in IMHA.
What is a prozone effect?
The prozone effect is a phenomenon observed in highly positive samples. The high concentration of anti-erythrocyte antibodies inhibits the positive reaction. An example is pictured below (Fig. 6).
The EDTA-blood sample presents a blood clot, can the Coombs’ test overcome this?
Unfortunately no. The presence of intact red blood cells is mandatory for the performance of a correct Coombs’ test. However, it is important to know the difference between a blood clot and an agglutination. The blood clot is the result of the physiological coagulation, and can occur when the sample is not correctly mixed with EDTA-anticoagulant. The blood clot is irreversible. To avoid this: after sampling, gently repeatedly invert the sample. The agglutination can be caused by different factors. In most cases, the agglutination is reversible, e.g. by warming up the sample in your hand, or by washing the cells.
-
Cocker Spaniels are among the breeds predisposed to IMHA.
Picture credits: envatoelements
-
Fig. 1: Schematic work-up of anemia.
PLEASE NOTE: Very early hemolysis may not yet or only slightly be regenerative
(bone marrow needs a few days to react). In addition, there are non-regenerative
forms of IMHA (formation of antibodies against erythrocyte precursors).
Picture credits: Dr Jennifer von Luckner
-
Fig. 2: Possible causes of hemolysis.
Picture credits: Dr Jennifer von Luckner
-
Fig. 3: Sample material to submit when IMHA is suspected.
Picture credits: Laboklin
-
Fig. 4: Blood smear from a dog with IMHA showing spherocytes, anisocytosis and
polychromasia.
Picture credits: Dr Nadine Idalan
-
Fig. 5: The Coombs’ reagent (shown in purple) induces an agglutination when anti-erythrocytic antibodies are present on the surface of the red blood cells.
Picture credits: Dr Nadine Idalan
-
Fig. 6: Coombs’ tests performed with the microtiter plate method. The titers are read from the left (low titers) to the right (high titers up to 1:2048). The last row only contains a mixture of NaCl and blood cells with no reagent and is used as negative auto-control. The titers below 1:8 are considered negative.
The first line is a negative sample (DAT-), the second line is a positive sample with the titer 1:32 (DAT+), on the last line the titers 1:2 to 1:16 are negative (prozone effect), however this sample is strongly positive (1:2048).
Picture credits: Dr. Nadine Idalan et al.
-
Fig. 7: Autoagglutination in an EDTA tube before washing.
Picture credits: Dr Nadine Idalan
Autoagglutination in my sample: Can it still be tested?
The erythrocytes are washed prior to the Coombs’ test. Despite autoagglutination, it is therefore possible to perform a Coombs’ test on the majority of these samples. A rare exception: If autoagglutination persists after washing, the result of the Coombs’ test cannot be read.
My sample shows autoagglutination: Is a Coombs’ test necessary, or is the agglutination enough to make a diagnosis?
One must differentiate between persistent autoagglutination after washing and an autoagglutination before washing the red blood cells. In many cases, the agglutination before washing is not diagnostic. Persistent autoagglutination is however strongly suggestive for IMHA. Our laboratory report will inform you about the persistent autoagglutination in your sample.
I have already started immunosuppressive treatment: Is it still meaningful to order a Coombs’ test?
The Coombs’ test can remain positive for up to 24 weeks after treatment despite immunosuppressive medication. A negative result, however, does not exclude IMHA.
I have already evaluated the blood smear under the microscope and found spherocytes: Do I still need to perform a Coombs’ test or can I already diagnose IMHA?
Spherocytes can be seen in small quantity in healthy dogs, and in moderate quantity in other diseases (zinc intoxication, poisoning, DIC…). However, five spherocytes per visual field at 100x magnification are considered supportive for IMHA. Hereditary spherocytosis is an important but very rare differential diagnosis. Please note that cats physiologically have round erythrocytes without central pallor, which makes the evaluation of spherocytes in cats unreliable.
I already tested my patient, the Coombs’ test titer was high, what does it mean?
High and low titers have the same meaning: the erythrocytes are coated with auto-antibodies. So far, there are no proof – in human and veterinarian medicine – that a higher titer correlates with stronger anemia, hemolysis or worse prognosis.
Dr Nadine Idalan, Dr Maria Brockmann
Further reading:
-
Garden OA, Kidd L, Mexas AM, Chang YM, Jeffery U, Blois SL, Fogle JE, MacNeill AL, Lubas G, Birkenheuer A, Buoncompagni S, Dandrieux JRS, Di Loria A, Fellman CL, Glanemann B, Goggs R, Granick JL, LeVine DN, Sharp CR, Smith-Carr S, Swann JW, Szladovits B. ACVIM consensus statement on the diagnosis of immune-mediated hemolytic anemia in dogs and cats. J Vet Intern Med. 2019; (2):313-334.
-
Idalan N, Zeitz JO, Weber CN, Müller E, Giger U. Comparative study of immunohematological tests with canine blood samples submitted for a direct antiglobulin (Coombs‘) test. Canine Med Genet 2021;8(1):10.