Alopecia (hair loss) in cats is a common reason for cats being presented to the veterinary practice. First of all, it must be clarified whether the alopecia is pathological hair loss. Owners are often concerned in cases of pronounced coat shedding, but as long as there are no signs of alopecia or other clinical signs (e.g. pruritus), the hair shedding should be considered physiological. In Persian cats, even focal alopecia may occur intermittently during the shedding period. There are also alopecias/hypotrichosis that are not pathological in certain breeds or specific locations, e.g. alopecia in sphynx cats, alopecia of the pinnae in older Siamese cats, or variable degree of alopecia in the preauricular region in all cat breeds.
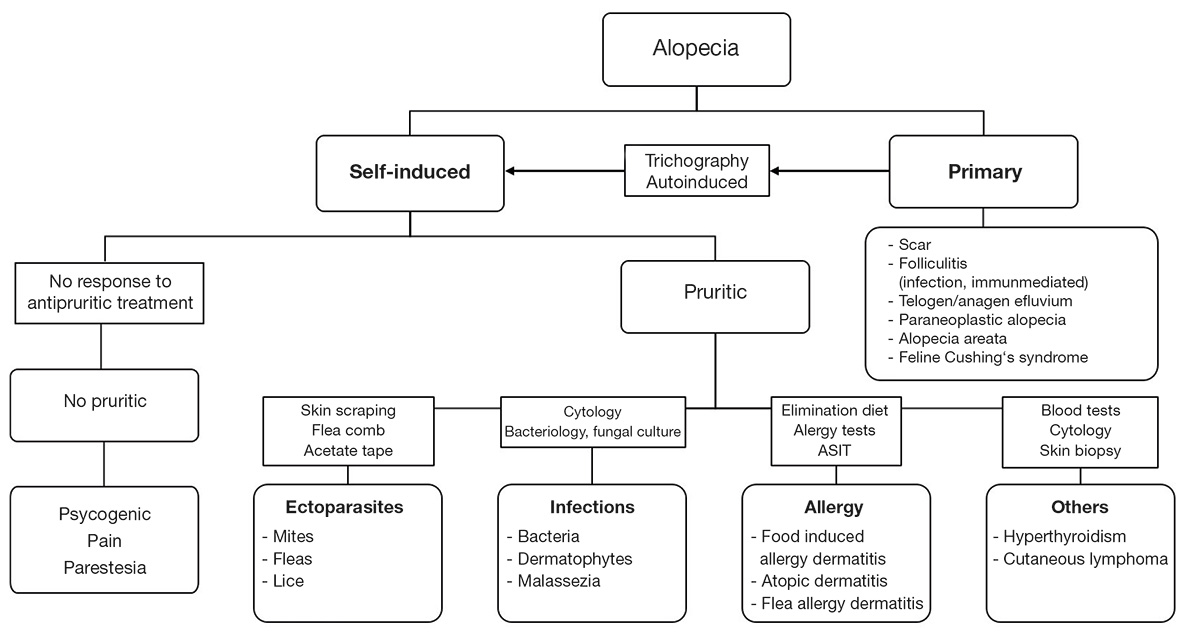
If pathological alopecia is present, various differential diagnoses are possible. Therefore, it is advisable to examine animals with alopecia – like all dermatological patients – according to a defined diagnostic protocol. The first step is always to obtain a detailed clinical history. A pre-printed formulary, which the owner may fill out in advance (waiting room), can always help. Based on this information, such as the age of the patient, what exactly were the symptoms like at the beginning of the problem (which came first: the alopecia or the itching?), illness of cohabiting animals or skin changes in humans, essential clues can already be gained for drawing up, after the clinical exam, a differential diagnosis list. Clinical examination is followed by a detailed dermatological exam, checking the patient’s skin from the nose to the tip of the tail for the presence of any lesion. For the systematic diagnostic work-up, it is helpful to divide the possible causative diseases into ”self-induced” and ”spontaneous” alopecias (Fig. 2). Some disorders can manifest in both forms (e.g. dermatophytosis, cutaneous lymphoma). In these cases, on the one hand, there is damage to the hair follicles causing hair loss, but at the same time, there is itching (e.g. due to secondary infections in dermatophytoses) leading to self-induced or secondary alopecia (see fig. 2).
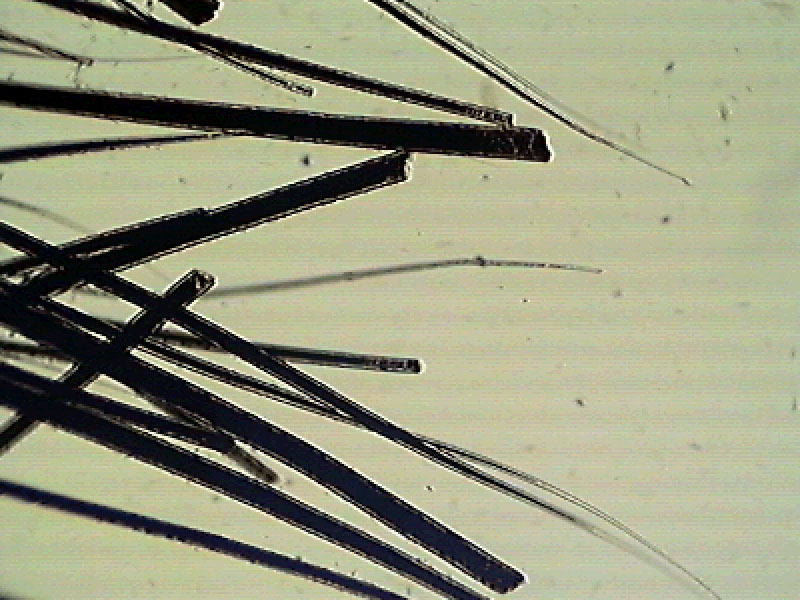
The diagnosis of self-induced alopecia is easy to make in animals that show increased grooming. However, many cats tend to practise this intensive grooming only in the absence of their owners. The visualisation of broken hairs by trichography suggests self-induced alopecia by licking (see fig. 3).
Pruritus is the most common cause of alopecia in the cat, in adult cats this is usually related to allergic diseases. However, before starting an allergy workup, the presence of infections or infestations must be excluded. Therefore, the first step is to detect or exclude ectoparasites through a flea comb, superficial/deep skin scraping and possibly adhesive tape. Fleas, lice, Cheyletiella mites, Otodectes mites (can also leave the ear canal) and Notoedres mites produce pruritus. Infestation with the mite Demodex gatoi, which does not live in the hair follicles but in the stratum corneum, is intensely itchy, unlike other species of Demodex. Fleas can additionally induce a hypersensitivity reaction. Even if no parasite infestation can be proven, patients with pruritus should receive continuous ectoparasite prophylaxis against flea and mite infestations (e.g. isoxazolines). In this way, flea allergy dermatitis can be diagnosed and treated at the same time. The next step is to check bacterial and fungal infections by cytological, bacteriological and fungal examination. Dermatophytes can be the cause of pruritic and non-pruritic alopecia. Bacteria and Malassezia generally represent secondary infections. If bacteria of the normal skin flora or Malassezia are cultured, the number of organisms can be assessed cytologically, whether it is only physiological colonisation, overgrowth or an infection. While Malassezia dermatitis is often found in dogs as a complication of allergies, it usually indicates more serious underlying diseases such as systemic infections or neoplasia in cats. Besides detecting infection, a cytological examination may suggest non-infectious diseases that can cause pruritus, such as pemphigus foliaceus or cutaneous lymphoma.
If an infection/infestation has not been diagnosed or if the clinical signs do not improve after appropriate treatment, the suspicion of an allergic disease comes to the fore. As it is impossible to distinguish clinically which type of allergy is involved, a food allergy should first be investigated through an elimination and provocation diet. During the elimination diet (8 – 12 weeks), a food with a single protein and carbohydrate source is fed. These can be ingredients that the animal has never eaten before if such can be identified, but food allergy testing is recommended, as a blindly selected diet runs the risk of not being tolerated. Based on the result, a protein source and a carbohydrate source are selected to which there is no positive test reaction in either the IgE or IgG antibody range. In general, the owners’ willingness to comply with a strict diet can also be increased if a written test result is available. In addition, compliance can still be improved by keeping a feed diary. Since several studies have found contamination of commercial diets with undeclared protein components, the elimination diet should ideally be home-prepared. If this is not possible, a high quality (peptide size < 1 kDa) hypoallergenic or hydrolysed veterinary diet (not supermarket or internet feed) should be used.
-
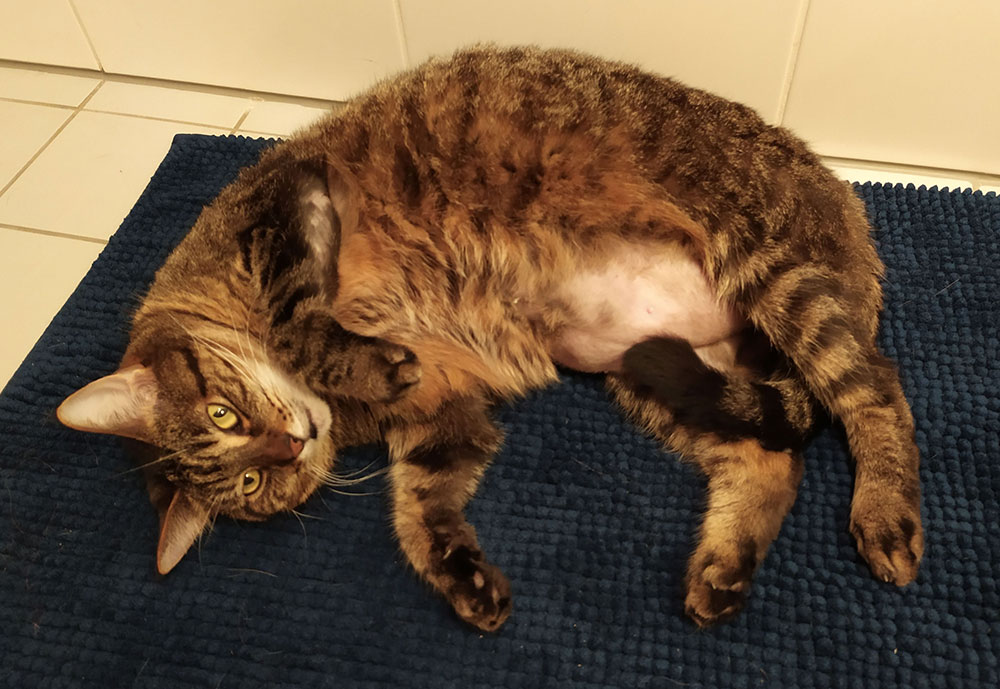
Fig. 1: Self-induced bilateral symmetric alopecia on the abdomen
Source: Elisabeth Steinkress
- Fig. 2: Diagnostic algorithm for feline alopecia
-
Fig. 3: Trichography – broken hair tips
Source: Dr Regina Wagner
-
Fig. 4: Alopecia with crusts – food induced allergy dermatitis
Source: Dr Maria Christian
-
Fig. 5: Pemphigus foliaceus
Source: Dr Ulrike Wurm
Suppose adherence to the strict diet for at least eight weeks does not result in a satisfactory improvement of the pruritus. In that case, the differential diagnosis of allergy to environmental allergens (FASS according to the new nomenclature = feline atopic skin syndrome) comes into focus. FASS diagnosis is always clinical based on a detailed clinical history, the clinical exam, and the exclusion of other pruritic diseases. Allergy tests (intradermal test or serological IgE detection using the FcEpsilon receptor test®) are not diagnostic tests but serve to identify the triggering allergens. There is the possibility to test reactions to allergen groups such as mites, pollens, fungal spores and flea saliva in a screening test. If there is a strong clinical suspicion of flea allergy, the test for flea saliva IgE can also be carried out as a single test. Subsequently, the positive allergen groups can be differentiated through main tests (pollen = seasonal allergens; mites and fungal spores = annual allergens). Furthermore, it is possible to detect allergen-specific antibodies (IgE) against less common allergy triggers such as insects or epithelia/feathers of various animal species. For patients who live in or regularly travel to the Mediterranean region, a specially developed panel is available, which considers the flora of southern Europe. If an allergy to Malassezia is suspected, Malassezia IgE can be determined. Based on the findings, a solution for allergen-specific immunotherapy can finally be prepared. This hyposensitisation is a lifelong therapy. A handy tool to never miss an injection appointment is Laboklin’s new 4Paws app for veterinarians and pet owners, which can be installed free from app stores. It also reminds the pet owner of vaccination appointments and the administration of other medications, ensuring compliance with the treatment plan.
More rare causes of self-induced pruritic alopecia include hyperthyroidism and cutaneous lymphoma. In older cats showing other clinical signs of hyperthyroidism, total serum thyroxine should be determined before allergy testing. In the case of cutaneous lymphoma, cytological examination may provide clues to this diagnosis which should be complemented by biopsy for diagnosis.
Non-pruritic self-induced alopecia occurs much less frequently than the pruritic form. It may be caused by ”psychological illness”, pain or neurological disorders/paraesthesias. Psychogenic alopecia can be triggered by stress factors such as moving house, loss of partner animal or caregiver, new family members, etc., while pain and paraesthesias can be the result of trauma, musculoskeletal disorders or neuropathies. A suggestive diagnosis is made when patients with increased grooming do not respond to antipruritic therapy. However, all causes of pruritic alopecia must first be ruled out. In a study of 21 cats examined for psychogenic alopecia, alopecia was due to a purely behavioural problem in only two animals. All the others had at least one other additional disease, such as food allergy and atopy, which explained the intense grooming behaviour (Waisglass et al., 2006).
Primary alopecia is very rare compared to self-induced alopecia. A diagnostic clue for primary hair loss is when hair can be plucked easily from the edges of the lesions. The first thing to check is whether the alopecic areas may be scars (e.g. trauma, repeated glucocorticoid injections). A relatively common cause is folliculitis resulting from demodicosis, dermatophytosis or bacteria, but also immune-mediated diseases (e.g. pemphigus foliaceus, Fig. 5). The hair follicle is damaged by inflammation, and the hair falls out. After intense psychological or even physical stress, anagen (after a few days) or telogen (after 1 to 3 months) effluvium can cause diffuse, non-inflammatory alopecia. Especially in older animals, alopecia can occur in the course of neoplastic diseases (liver and bile duct carcinoma, pancreatic carcinoma), which mainly manifests itself on the abdomen in the form of complete alopecia, shiny and waxy skin. These animals usually also show systemic clinical signs. The diagnosis is confirmed by imaging techniques and histopathological examination of the tumours. Alopecia areata is a rare form of alopecia in cats, leading to hair loss due to autoimmune destruction of hair follicles. Diagnosis is made by histopathological study. Feline Cushing’s syndrome is also a sporadic disease. In addition to alopecia and thin, fragile skin, affected animals often present with polydipsia/polyuria, polyphagia, a pendulous abdomen and, in about 80% of cases, poorly regulated diabetes mellitus. Diagnosis is made by appropriate serum-based functional tests (e.g. dexamethasone suppression).
Dr. med. vet. Maria Christian