Strangles is caused by the gram-positive, β-haemolytic bacterium Streptococcus equi subspecies equi. After an incubation period of up to 14 days, severe courses of the disease are possible, especially in young horses. The exact duration before the onset of the first clinical signs depends on the individual immunity of the affected horse and the pathogen load. Adult animals may show an atypical clinical picture with a rather mild course of disease without lymphadenopathy. Shedding of the pathogen usually begins 2 – 3 days after the onset of fever and typically lasts 2 – 3 weeks.
Initially, the infection presents with non-specific signs such as fever (up to 42 °C), lethargy, anorexia and cough. After contact with the mucous membranes of the upper respiratory tract, direct bacterial colonisation of the lymphoid tissue of the pharynx, the retropharyngeal lymph nodes and subsequently the mandibular and suprapharyngeal lymph nodes occurs. The antiphagocytic properties of the bacteria lead to the typical abscess formation caused by accumulated neutrophils. These abscesses usually rupture 7 – 10 days after infection and drain the pus directly to the outside or into the upper respiratory tract and the guttural pouches, so that purulent, unilateral or bilateral nasal discharge can occur.
Depending on which lymph nodes are primarily affected, there may not always be swelling visible from the outside. Severely enlarged lymph nodes and inflammation of the pharyngeal mucosa may cause obstruction of the upper respiratory tract as well as dysphagia and even partial laryngoplegia.
- Photo credits: Fotolia
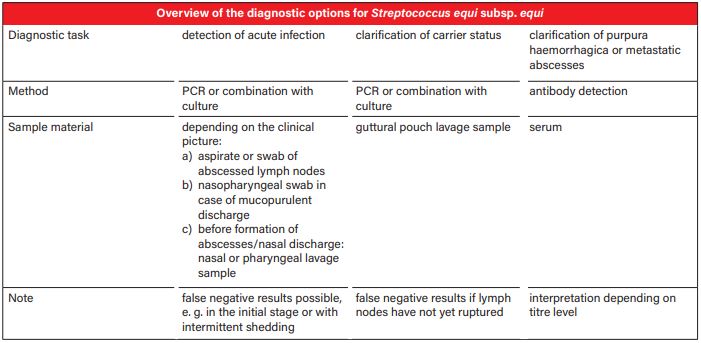
- Tab. 1: Overview of the diagnostic options for Streptococcus equi subsp. equi
Rupture of retropharyngeal lymph node abscesses into the guttural pouches can result in empyema if drainage is insufficient and chondroids may form if pus remains for a longer period of time. In these cases, horses may be persistently infected for years and shed the pathogen intermittently. Prevalence for this is about 2 – 10% of the animals affected in an outbreak. Streptococcus equi subsp. equi can spread to all organs via haematogenous or lymphogenous routes and lead to purulent inflammation or abscesses (“bastard strangles”). Another possible complication is purpura haemorrhagica (petechial fever, morbus maculosus).
After overcoming the disease, most horses develop long-lasting immunity, but reinfections have also been reported. As the pathogen is highly contagious, it can spread rapidly throughout the entire herd via direct and indirect transmission (e. g. water troughs, people, insects). Although the tenacity of the strangles pathogen in the environment is rather low, survival in water is reported to be up to 4 – 6 weeks. Especially silent carriers can considerably promote the spread of the bacteria. For newly added horses, a quarantine of at least 3 weeks including testing for Streptococcus equi subsp. equi is recommended in order to identify silent carriers. Because of the delayed shedding of the pathogen, it is possible to protect other horses from infection if there is an outbreak in the herd by isolating febrile horses early on. Shedding of the pathogen can continue for up to 3 – 7 weeks after the acute phase of the disease has subsided and can also lead to intermittent shedding if the bacteria retreat into the guttural pouches or the paranasal sinuses. If the mucopurulent nasal discharge persists for more than 2 weeks, endoscopic examination of the guttural pouches is indicated.
Testing for carrier status is recommended at the earliest 3 weeks after the cessation of clinical signs or the last contact with an infected horse.
Detecting these silent carriers with intermittent shedding, which are the reservoir for new outbreaks, is crucial for the management of strangles.
This Laboklin aktuell is meant to provide you with an overview of the diagnostic options and to support you in choosing the appropriate sample material and most useful detection method for the different diagnostic tasks.
Direct pathogen detection
Sample material
The best sampling method, the success of direct pathogen detection and the interpretation of laboratory findings depend on the epidemiology of the pathogen. At the beginning of the disease, Streptococcus equi subsp. equi infects the lymphoid tissue quite quickly and cannot or hardly be detected on the mucous membranes at this time. Especially in the first 2 – 3 days after the onset of the first non-specific signs (fever), there is no shedding of pathogens. Negative PCR or culture tests are therefore not diagnostically conclusive for the absence of bacteria, particularly at an early stage. Especially if there is a strong suspicion of strangles and pathogen detection has been negative, another sample should be submitted and, if necessary, the choice of sample material should be reconsidered.
Sample collection depends on the clinical signs and symptoms. If there are abscessed lymph nodes, a swab may be taken from the aspirate or abscess material. Nasopharyngeal or deep nasal swabs are the most suitable sample material for horses with mucopurulent nasal discharge. If the horse does not yet show any of these signs, it is recommended to collect nasal or pharyngeal lavage samples if strangles is suspected. This increases the probability of detection, as a larger mucosal surface is indirectly sampled here. In order to exclude carriers, a guttural pouch lavage should be chosen. Sensitivity of pathogen detection increases with repeated testing. It is recommended to take up to 3 samples at weekly intervals before declaring horses as pathogen-free.
PCR
Realtime PCR is ideally suited for direct pathogen detection thanks to its high sensitivity and specificity combined with only a short processing time. Thus, PCR testing of guttural pouch lavage samples is considered the gold standard for the identification of clinically healthy carriers. However, it should be noted that false negative results may be possible if the retropharyngeal lymph node abscesses have not yet ruptured into the guttural pouches. For PCR tests from swabs, (moistened) swabs without medium should be used. The detection of specific gene sequences allows to differentiate between Streptococcus equi subsp. equi and Streptococcus equi subsp. zooepidemicus. At Laboklin, it is possible to choose between a single determination of the strangles pathogen or the detection of both subspecies mentioned above. An infection with the facultative pathogenic commensal Streptococcus equi subsp. zooepidemicus cannot always be clinically distinguished from strangles, especially in foals and young horses. Thus, this double determination allows for a comprehensive work-up of suspected cases of strangles. As PCR does not differentiate between living and dead microorganisms, positive results can be confirmed by culture.
Culture
For growing a culture, it is important to send in an (additional) swab with medium. In conventional bacteriology, both subspecies are detected (Streptococcus equi subsp. equi and Streptococcus equi subsp. zooepidemicus) and differentiated by MALDI-TOF. Compared to PCR, culture has a lower sensitivity, which is why it is no longer considered the gold standard for pathogen detection. There is a risk of false negative results, especially during the incubation period, at the onset of clinical signs, if pathogen shedding is low and in case of pre-treatment with antibiotics. However, it should be emphasised that culture confirms living microorganisms capable of reproduction and is a rather inexpensive way of testing. Moreover, the option of doing an antibiogram only exists here. In general, however, β-haemolytic streptococci do not tend to develop any resistances. (Tab. 1)
Indirect pathogen detection
Serology
The test Laboklin uses focuses on the quantitative detection of antibodies against the surface antigen SeM, a virulence factor of Streptococcus equi subsp. equi. Cross-reactivity with antibodies against Streptococcus equi subsp. zooepidemicus cannot be completely ruled out. The highest titres can be expected approx. 5 weeks after exposure and they will also remain high for at least 6 months. To clarify acute infections, pathogen detection should always be preferred to testing for antibodies. Serology is mainly used in horses with suspected purpura haemorrhagica or metastatic abscesses. Determining the titre can also be useful before vaccinating against strangles. Yet, vaccination titres cannot be distinguished from infection titres.
Serological results should be interpreted as follows:
- Recent infection: at least 4-fold titre increase in paired serum (10-day interval).
- Titre ≥ 12800: supports the diagnosis of Streptococcus equi subsp. equi-associated purpura haemorrhagica or metastatic abscesses
- Titre ≥ 3200: increased risk of developing purpura haemorrhagica when vaccinated against strangles
- No conclusion on the protection of the patient can be drawn from the titre level
- No interpretation regarding carrier status
Abnormal laboratory parameters in case of strangles
Horses suffering from strangles often show leukocytosis with neutrophilia as well as highly elevated acute-phase proteins (e. g. SAA, fibrinogen). Prolonged cases of the disease may be accompanied by anaemia.
Conclusion
In summary, the various tests form the basis for diagnosis, management or prevention of outbreaks in a herd. Each of the available tests can provide specific information. Therefore, depending on the diagnostic task, a combination of several test methods or repeated sampling may be useful.
Dr. Clarissa Jung, Dr. Svenja Möller