Throughout the season (spring – autumn), the ovaries in horse mares show physiologically cycle-related changes (development of follicles, ovulation, formation of Corpora lutea).
Corresponding to the hormonal changes especially during estrus, mares can show behavioural changes that are not observed during dioestrus or anoestrus (e.g. frequent urination, sensitivity to thigh pressure, flashing).
Pathological changes in the ovaries can lead to striking clinical symptoms depending on the type and severity. The most common reasons for the clinical presentation of such mares are rideability problems or abnormalities in the behaviour of the animals, such as stallion behaviour, biting, striking, mounting or aggressiveness towards other horses and humans. Furthermore, cycle disorders or acyclia can lead to sub- or infertility and thus to economic losses on the studs.
A careful general and clinical-gynecological examination (including ultrasound if necessary) of the mare is important for the diagnostic work-up of such cases in order to rule out extragenital causes for the symptoms described above (e.g. trauma to the musculature, spinal and muscle diseases, stomach ulcers, dental diseases).
The average size of active ovaries in warmblood mares is approx. 6-8 cm from cranial to caudal and 3-4 cm in diameter. If asymmetry with unilateral megaovary or pain on palpation can be detected pathological changes should be considered in addition to the physiological pre-ovulatory (Graafian) follicles or corpus luteum.
- Image source: Adobe Stock
-
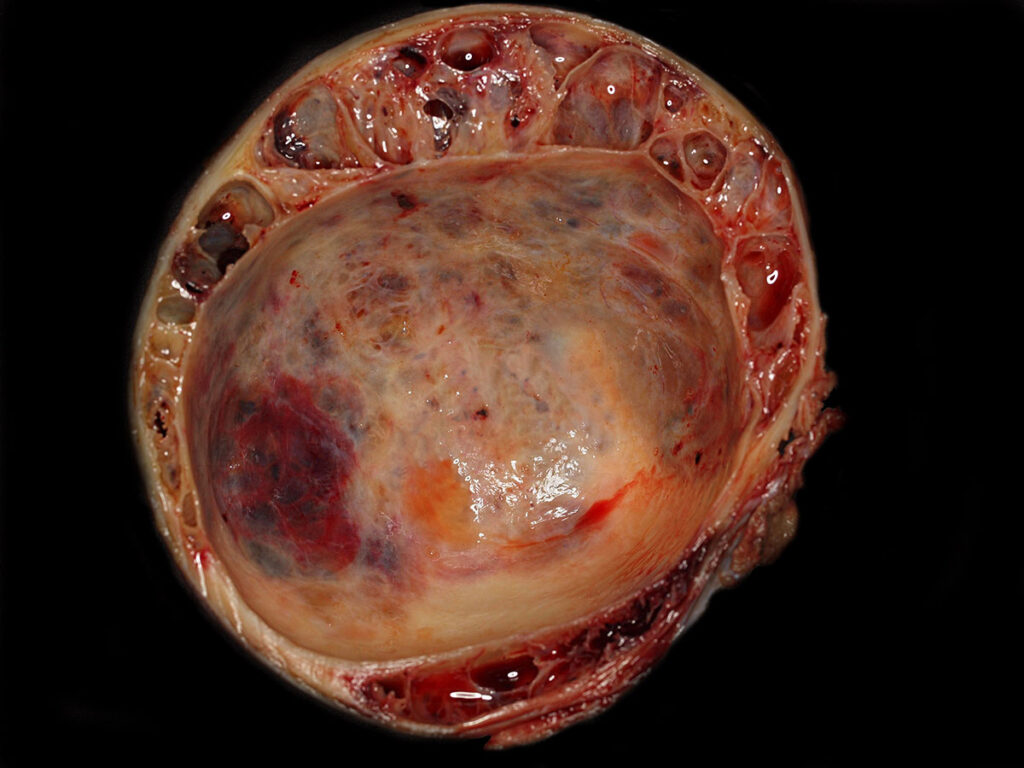
Fig. 1: Granulosa cell tumour with honeycomb structure in the marginal area and formation of a large central cyst.
Image source: Laboklin
Some diseases can be diagnosed in the laboratory by means of serological tests, while lesions that are not accompanied by specific changes in the blood or hormone levels can only be clearly characterised by histopathological examination.
The most important neoplastic change in the equine ovary is the granulosa cell tumour (GCT), as this neoplasm is by far the most common in mares. These are tumours that arise from the follicular granulosa cells and (more rarely) also contain a cellular component of the theca cell layer (granulosa-theca cell tumours). Classic findings in the anamnesis are cycle and/or behavioural abnormalities and asymmetry of the ovaries. On sonographic examination, the enlarged ovary (Fig. 1) may appear as a honeycomb-like structure, solid or as a single large cystic structure.
Various indicators are used in equine reproductive medicine to diagnose hormonally active ovarian neoplasia, whereby the serological determination of anti-Müllerian hormone (AMH), which is tested daily at Laboklin, has proven to be the most sensitive marker. In the mare, the hormone is produced in the granulosa cells of pre-antral and antral follicles and is not subject to cyclical or gravidity-related fluctuations. The serum concentration is increased up to 20-fold in the presence of GCT. In rare cases, AMH can provide ambiguous values (e.g. in the early stages of a neoplasia or in the case of follicular cysts). In such cases, a follow-up examination in 2-4 weeks is recommended.
Furthermore, clinical and serological diagnostics can be supplemented by measurement of the peripheral sex steroids oestradiol and testosterone. Both hormones are produced in the granulosa and/or theca cells of the Graafian follicle and can show highly elevated levels in the presence of GCT. However, it should be noted that the sex steroids have a significantly lower sensitivity than AMH, as hormonally inactive GCTs can also develop.
Progesterone is unsuitable for the serological diagnosis of ovarian GCT, as it is produced in the cells of the corpus luteum and therefore normal to low values are to be expected.
Another laboratory diagnostic method that (in addition to other information) also provides an indication of the presence of endocrine active ovarian dysfunction is the histological examination of an endometrial biopsy. The atypical hormonal activity results in irregular endometrial differentiation, which is morphologically detectable. It is important to note that this endometrial maldifferentiation is not specific for the presence of a granulosa cell tumour and is therefore not included in the categorisation according to Kenney & Doig (1986) mod. according to Schoon et al. (1992), although endometrial maldifferentiation can reduce fertility.
Thecomas, follicular (lutein) cysts or ovarian stromal hyperthecosis as well as other endocrine imbalances can also be associated with endometrial maldifferentiation. Therefore, it is crucial to consider the medical history and the results of the clinical gynaecological and serological examinations for the final interpretation.
All other primary or metastatic tumours of the ovary, such as carcinomas or dysgerminomas, are endocrinologically inactive and therefore show no specific clinical-chemical abnormalities. The final diagnosis in such cases requires a histopathological examination after removal of the ovary (ovariectomy). It is crucial to send the entire ovary for examination in order to obtain a representative sample for diagnosis.
In addition to tumorous changes in the ovary, there are also non-neoplastic diseases that are more challenging to diagnose. These diseases often show no specific clinical symptoms and cannot be clearly identified by laboratory diagnostic tests.
Anovulatory haemorrhagic follicles (AHF) occur specifically during the transition cycles in autumn and spring, when ovulation fails.
However, if AHFs occur during the physiological breeding season, they must be considered pathological findings as the interovulatory period can extend up to several months under certain circumstances. Gravidity is not possible in this case. In laboratory diagnostics, progesterone levels >1 ng/ml can often be measured in the serum in the presence of AHF, which indicates the presence of luteinised tissue. It should be noted that low values do not rule out the presence of AHF.
Postovulatory haematomas are sometimes observed in older mares. Depending on their size, they can be accompanied by pain, colic and bleeding into the surrounding tissue, anaemia and reduced performance. Laboratory diagnostics usually do not show any specific changes in the blood count, as anaemia, for example, can also have other causes – the coagulation status should be checked if necessary.
Abscesses of the ovaries may be caused by septic processes ascending from the uterus or salpinx or injuries/manipulations, resulting in clinical symptoms such as fever, colic, anorexia and apathy. Laboratory diagnostics may reveal leucocytosis and an increase in inflammatory parameters. If the process spreads to the peritoneum, this can be demonstrated in a cytological and physical-chemical examination of abdominal cavity fluid. A neutrophilic cell picture with a massively increased cell count and increased protein content and evidence of bacteria can be expected, as can also be seen in intestinal torsion. At the same time, a bacteriological examination of native material is recommended.
In contrast to ruminants, ovarian cysts rarely occur in mares and are usually endocrinologically inactive. Most commonly, inclusion cysts are seen. These cysts can develop after hematomas or result from dislocation of surface epithelium in the course of numerous ovulations as the mare ages. As the area of the ovulation fossa in the equine ovary is predisposed to the development of these cysts, they are most frequently detected in this area. In most cases, these inclusion cysts do not lead to a decline in fertility, but in rare cases they can cause an obstruction of the infundibulum so that the oocyte cannot pass through this mechanical obstacle after the follicle has ruptured.
Histologically, these inclusion cysts can be differentiated according to their localisation into fossa cysts and fimbrial cysts. These structures have no hormonal activity.
Follicular cysts develop from Graafian follicles that are in the process of forming and are characterised by a lining of granulosa cells. If ovulation fails haemorrhagic follicles may develop (see above), which can result in an increase in the serum concentration of progesterone.
Furthermore, cysts in other locations can be classified as ovarian cysts or paraovarian cysts.
Although all these cystic structures can reach a considerable size in individual cases (up to 20 cm in diameter), they are usually changes without clinical relevance that are diagnosed incidentally.
Conclusion
- Heterogeneous clinical picture of ovarian changes in the mare, laboratory diagnostic work-up supports the clinical diagnosis.
- Serological diagnostics to clarify a granulosa cell tumour in megaovaries: Measurement of serum AMH concentrations (CAVE! submission of cooled serum!), supplemented by oestradiol and testosterone if necessary.
- Histological examination of an endometrial biopsy for evidence of endocrine dysfunctions.
Dr. Kathrin Jäger
Range of services
- Oestradiol
- Testosterone
- Progesterone
- Anti-Müllerian hormone
- Pathohistology