Feline asthma belongs to the feline atopic syndrome (FAS), including other allergic diseases such as feline atopic skin syndrome (FASS). FASS presents with skin reaction patterns such as miliary dermatitis, eosinophilic granuloma complex, self-induced alopecia and head/neck pruritus. This nomenclature of feline allergic diseases has only recently been established. Feline asthma is a chronic disease with an eosinophilic inflammatory reaction to inhalant allergens. This reaction affects the bronchioles and leads to spontaneous and reversible bronchoconstriction, which manifests as acute dyspnoea or chronic cough and expiratory dyspnoea (1).
Pathogenesis
Asthma is a relatively common inflammatory disease of the lower respiratory tract (according to literature, it affects 1 – 5% of the feline population). Affected cats are predominantly young, with the average onset age of symptoms between 0.5 and 4.5 years (2, 3). The similarity of feline asthma to human asthma is very strong, making the cat a model for human studies. Much of the information on this disease‘s pathogenesis, diagnosis, and therapy have been derived from these allergen-induced experimental models. Feline asthma is caused by a type 1 hypersensitivity reaction to aeroallergens (house and storage dust mites, pollen, fungal spores, animal dander). It leads to activation and differentiation of allergen-specific TH2 cells, which trigger an inflammatory reaction and IgE production. After sensitisation, repeated inhalation of allergens causes clinical signs. IgEs bound to mast cells, and basophil granulocytes are activated by the allergen and lead to degranulation, an inflammatory cascade is triggered, and eosinophil granulocytes migrate to the lungs (4). These immunological reactions lead to chronic airway inflammation, dominated by eosinophils in the long term.
Thickening of the airway epithelium, metaplasia and mucosal damage occurs. Hyperexcitability and obstruction of the bronchi lead to valve function and thus to so-called “air trapping”: air can no longer escape during expiration, and life-threatening bronchospasm can be triggered (3).
Clinical signs
Clinical signs of feline asthma are acute or chronic. A cat with asthma may present with acute respiratory signs such as dyspnoea, mouth breathing, hyperpnoea, tachypnoea, collapse and pale or cyanotic mucous membranes. Chronic signs include dyspnoea, expiratory wheezing breath sounds, chronic coughing (often misinterpreted as retching) and exercise intolerance. In some cats, the only clinical sign is a chronic cough. Exercise intolerance usually occurs in young and active cats. On auscultation, expiratory wheezing and cracklin breath sounds are typically heard (2, 3).
-
Fig. 1: Typically stretched head and neck posture of a coughing cat.
Source: Dr Elisabeth Reinbacher
- Fig. 2: Diagnostic tests in feline asthma
-
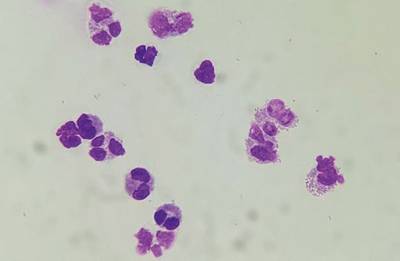
Fig. 3: Eosinophils on cytological examination of a BAL sediment smear
Source: Dr Maria Christian
-
Fig. 4: Aelurostrongylus abstrusus larvae in a sediment smear of a BAL.
Source: Dr Maria Christian
Diagnosis
There is no single specific test to diagnose feline asthma. Diagnosis is made based on a detailed history, clinical signs, chest radiographs and bronchoalveolar lavage (BAL), with cytological and microbiological examinations (Fig. 2). Unlike in human medicine, lung function measurements such as spirometry and plethysmography are rarely used to diagnose and monitor feline asthma due to a lack of (technical) availability and scientific data. Biomarkers (e.g. measurement of cysteinyl leukotrienes used in humans with asthma for diagnosis and therapy monitoring) have only been used in cats in experimental studies (2, 3). Further studies should demonstrate whether these biomarkers can be used meaningfully for diagnostics in clinical practice in the future (5). The principal differential diagnoses are chronic bronchitis, respiratory tract parasites, heart disease, pneumothorax, pleural effusion, neoplasms, foreign bodies, and bacterial and viral infections (2, 3). Feline chronic bronchitis must be differentiated from feline asthma. It is caused by previous infections or inhaled irritating substances from smoke or air pollution and differs from feline asthma not only in the cause but also in clinical course and treatment (3, 4). Cytological examination of the material obtained by BAL is essential to differentiate asthma from chronic bronchitis and underlying infectious causes. If the cat is on glucocorticoid therapy, it is recommended that the cat be weaned off at least 48 hours before the examination. BAL is performed by bronchoscopy or blind. The collected sample should be refrigerated until processing and low-speed centrifuged within a few hours to immediately prepare sediment smears. While neutrophilic granulocytes dominate chronic bronchitis, asthma is characterised by eosinophilic inflammation. If more than 20% of the cells (6) are eosinophilic granulocytes (although study results differ here), this is referred to as bronchial eosinophilia (Fig. 3).
An examination for mycoplasma is recommended using PCR testing. However, the clinical significance of mycoplasma in feline bronchial disease is not yet fully understood. Purely viral pneumonia is very rare in cats, but caliciviruses and feline herpesviruses can cause it and can be detected by PCR. Asthmatic cats often show eosinophilia on haematological examination. Furthermore, a faecal exam should be carried out to exclude an infestation with lung parasites. The Baermann-Wetzel method is the method of choice for detecting Aelurostrongylus abstrusus, the most relevant lungworm in cats in Central Europe (Fig. 4). Due to the intermittent shedding of larvae, a pooled stool sample increases the diagnostic significance. Faecal flotation to detect other lung parasites (e.g. Capillaria aerophilia) and migrating larvae (e.g. Toxocara cati) is also recommended (2, 3). In addition, in endemic areas, Dirofilaria immitis infection should be excluded. Since a negative coprological result does not exclude infestation due to intermittent parasite excretion, empirical antiparasitic treatment is recommended (5).
Allergy testing is indicated to identify the triggering environmental allergens and initiate allergen-specific immunotherapy (ASIT, hyposensitisation). Intradermal and serological allergy tests are available. Many veterinarians prefer serological allergen-specific IgE testing in the cat because it is easier to perform, and the results of an intradermal test are more challenging to interpret due to the weak reactions in this specie. Serological allergy tests (ELISA) detect the presence and amount of circulating allergen-specific IgE antibodies. An experimentally induced asthma study in cats showed that the serological test with the Fcε receptor has a high specificity compared to the intradermal test and is suitable for selecting antigens for ASIT (7). Laboklin uses the Fcε receptor in the test (2, 3). The recommended withdrawal periods before serological allergy testing should be taken into account: for oral glucocorticoids, eight weeks, inhaled glucocorticoids 2 to 4 weeks, and glucocorticoids with depot effect 12 weeks (2, 3).
Therapy
Acute symptoms require emergency treatment and usually respond well to combined therapy with glucocorticoids, bronchodilators and oxygen (2). Long-term symptomatic treatment of feline asthma is performed with glucocorticoids and bronchodilators administered systemically or by inhalation (8). Follow-up by repeated BAL cytology may be recommended to assess the success of therapy. However, symptomatic therapy does not prevent the immunological response and associated chronic remodelling processes that lead to impaired lung function. Therapeutic approaches that address the underlying immune-mediated pathology have been explored for several years (3, 5). Avoidance of the triggering allergens is undoubtedly the best of all therapies – but in most cases, not feasible. ASIT is recommended for the treatment of feline asthma. The therapy can prevent allergic reactions and induce immunological tolerance to the triggering allergens (5). ASIT is the only therapy that can causally intervene in pathogenesis. ASIT is an individual therapeutic solution composed of those allergens to which the cat has shown positive reactions in the allergy test and correlates with the previous report and clinical signs. It is applied subcutaneously at protocol-dependent intervals. Studies in experimentally induced asthma in cats suggest that ASIT can alleviate clinical signs and reduce the number of eosinophilic cells in the BAL (8). A clinical trial evaluating the effectiveness of ASIT for the treatment of feline asthma showed that 67% of cats with ASIT as sole therapy were asymptomatic. Improvement in clinical signs was reported in the remaining cats, which required additional glucocorticoids and bronchodilators 2 – 3 times weekly (9). Especially at the beginning of hyposensitisation, symptomatic medical treatment is often necessary, but it should be as low as possible so that the symptoms are not entirely suppressed but only alleviated. The ASIT therapeutic protocol sometimes has to be individually adapted the intensity of the clinical signs monitored. If symptoms are completely suppressed, the need to adjust the protocol may not be recognised. If hyposensitisation is successful, it should be continued for life. Cyclosporine, oclacitinib, antihistamines and essential fatty acids, such as those used in FASS, are poorly studied as therapies for asthma in the cat, there is currently insufficient data to recommend their use. Inhaled lidocaine, used in human asthma, or intravenously administered mesenchymal stem cells may be therapeutic approaches in the future (8).
Summary
Experimental studies have been instrumental in differentiating feline asthma from other lower respiratory tract diseases. Clinical studies, with more significant numbers of cases, investigating targeted therapies such as ASIT, focusing on the allergic cascade are scarce, but would be an essential basis for therapeutic options for feline asthma in the future.
Dr Elisabeth Reinbacher
Literature
-
Halliwell, R., Pucheu-Haston, C.M., Olivry, T., Prost, C., Jackson, H., Banovic, F., Nuttall, T., Santoro, D., Bizikova, P., Mueller, R.S.: Feline allergic diseases: introduction and proposed nomenclature.Vet Dermatol 2021, 32(1) 8-e2.
-
Santoro, D., Pucheu-Haston, C.M., Prost, C., Mueller, R.S., Jackson, H.: Clinical signs and diagnosis of feline atopic syndrome: detailed guidelines for a correct diagnosis. Vet Dermatol 2021, 32(1) 26-e6.
-
Grotheer, M., Schulz, B.: Felines Asthma und chronische Bronchitis – Übersicht zu Diagnostik und Therapie. Tierarztl Prax Ausg K Kleintiere Heimtiere 2019, 47(3) 175-187.
-
Halliwell, R., Banovic, F., Mueller, R.S., Olivry, T.: Immunopathogenesis of the feline atopic syndrome. Vet Dermatol 2021, 32(1) 13-e4.
-
Trzil, J.E.: Feline Asthma: Diagnostic and Treatment Update. Vet Clin North Am Small Anim Pract 2020, 50(2) 375-391.
-
Shibly, S., Klang, A., Galler, A., Schwendenwein, I., Christian, M., Guija, A., Tichy, A., Hirt, R.A.: Architecture and inflammatory cell composition of the feline lung with special consideration of eosinophil counts. J Comp Pathol 2014, 150(4) 408-15.
-
Lee-Fowler, T.M., Cohn, L.A., DeClue, A.E., Spinka, C.M., Ellebracht, R.D., Reinero, C.R.: Comparison of intradermal skin testing (IDST) and serum allergen-specific IgE determination in an experimental model of feline asthma. Vet Immunol Immunopathol 2009, 132(1) 46-52.
-
Mueller, R.S., Nuttall, T., Prost, C., Schulz, B., Bizikova, P.: Treatment of the feline atopic syndrome – a systematic review. Vet Dermatol 2021, 32(1) 43-e8.
-
Prost, C.: L’asthme félin: apport des tests allergiques et de l’immunothérapie spécifique. À propos de 20 cas, Revue Française d‘Allergologie et d‘Immunologie Clinique 2008, Volume 48 (5) 409-413.