Atopic patients often produce IgE against allergens. But there are some patients who despite presenting allergic clinical signs IgE cannot be detected; this disease is called atopic-like dermatitis (ALD). In human medicine, the condition is called intrinsic-atopic dermatitis (IAD).
Patients with ALD have negative results in allergy test, both in serological tests and in intradermal tests (IDT). This report explains what to consider for the diagnosis of ALD.
Clinical history
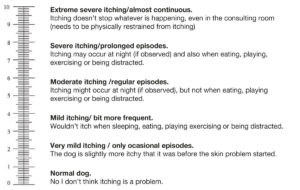
Rocky is a two-year-old male English Bulldog weighing 25kg, with a recurring history of otitis and pruritus with dermatitis all over the body for six months (Fig. 2). Rocky lives with his owner in an apartment. He is active and alert, eats and drinks normally and drops normal consistency stools 2 to 3 times a day. Rocky has been feed with several diets with pork, beef, lamb, rice, carrots, vegetables etc. An elimination diet with horse meat and potatoes was carried out, and no improvement was observed. The pruritus intensity is 8/10 without medication and 2-4 /10 with treatment, according to a Pruritus Visual Analog Scale (PVAS) (Fig. 1). From the beginning of the process, Rocky receives the following treatment: Prednisolone 12.5mg (0.5mg / kg) every 24h, weekly ear cleaning, weekly baths with chlorhexidine or Malaseb® shampoo and Bravecto® (Fluralaner) every three months as prophylaxis against ectoparasites. The owner does not want any further therapy with prednisolone.
-
Fig. 1: Pruritus Visual Ananlogic Scale for dogs (PVAS)
Rybnícek J, et al. Further validation of a pruritus severity scale for use in dogs. Vet Dermatol. 200920(2):115-22.
-
Fig. 2: Rocky
Picture Credits: Dr. Regina Wagner
Clinical examination
The dermatological examination revealed the presence of moderate to mild erythema on the muzzle, axillae, and abdomen. The interdigital and palmar areas of the front paws showed a moderate erythematous and exudative dermatitis. Between toes 3 and 4 of the front paws, there was mild alopecia with a moderate erythematous dermatitis. On the rear paws, the plantar area had mild erythema. The inner surface of the ears, as well as the entrance to the external otic canals, were erythematous. At otoscopy, both ear canals were moderately erythematous, stenotic and the eardrum was only partially visible.
In 2010, the Favrot criteria, with reasonable specificity and sensitivity for the clinical diagnosis of canine atopic dermatitis, were published. These criteria are based on the animal‘s clinical history and dermatological examination.
These criteria are:
- The appearance of the first clinical signs before three years of age
- Animals living mostly indoors
- Corticosteroid-responsive pruritus
- Primary pruritus, without lesions at the beginning of the process (pruritus sine materia)
- Chronic or recurrent yeast or bacterial infections
- Chronic or recurrent otitis externa
- The affection of front feet and ear pinna
- Non-affected ear margins
- Non-affected dorso-lumbar area.
At Rocky, most of the criteria were met.
Diagnostic tests
Cytology
Impression smears were taken from the muzzle, axillae, and abdomen. No bacteria or Malassezia were detected.
Cytology of the ears revealed the presence of neutrophils and cocci bacteria in moderate numbers.
Scotch tape cytology were obtained from interdigital and inter-pad spaces. Malassezia was detected on the tape.
In patients with chronic pruritus, sarcoptic mange is one of the differential diagnoses. However, Rocky received Bravecto® regularly and no other tests (superficial skin scraping) were performed.
Diagnostic and therapeutic plan
Treatment of Malassezia pododermatitis was started with baths with Malaseb® shampoo. External otitis was treated with Aurizon® ear drops (marbofloxacin, clotrimazole and dexamethasone) once a day for 14 days.
An elimination diet is the standard gold test for the diagnosis of food allergy. Rocky was not responding to the horse meat and potato elimination diet he was receiving. Although the diet was designed with a unique novel protein, and a unique carbohydrate source, there could be a cross-reaction problem between feed ingredients or diet errors (such as licking of dishes, eating food crumbles on the ground, or wrong food administration by other people). Therefore a second strict elimination diet with hydrolyzed feed (Anallergenic® of Royal Canin) was proposed for another eight weeks.
Prednisolone was tapered off from the fourth week of the elimination diet (the first week every two days, the second week every three days and then stopped). No improvement was shown under the new elimination diet, and a food allergy was excluded. A serological test for environmental allergens was performed.
Environmental allergen tests
Serology allergy tests are a reliable method to identify relevant environmental allergens for allergen-specific immunotherapy (ASIT) formulation. Dust and storage mites and pollens of grasses, herbs, and trees are the most common environmental allergens. But also, other allergens such as mould spores, insects and epithelia or feathers of animals can cause atopic dermatitis.
To perform an allergen test, the patient must not have received glucocorticoids for at least 12 weeks for injectable depot preparations, 6-8 weeks for oral administration, or 2-4 weeks for topical formulations (ear drops, creams, sprays). To avoid relapse of clinical allergy signs after the withdrawal of prednisolone and the elimination diet, Rocky received Lokivetmab (Cytopoint®) every four weeks.
According to the literature, Lokivetmab does not negatively influence allergy test results. Four months after prednisolone withdrawal, Rocky was tested against perennial, seasonal, epithelial, and animal feather allergens. The results of all the tests were negative. In animals with a clinical diagnosis of atopic dermatitis and negative result in one type of allergy test (serology or intradermal test), the employment of the other methodology is indicated. Rocky‘s intradermal test was also negative.
Diagnosis
Atopic-like Dermatitis (ALD)
Treatment
As the identification of allergen-specific IgE is not possible in atopic-like dermatitis, it is not feasible to formulate an ASIT in such patients. Hence, active and proactive therapy with anti-pruritic drugs like Prednisolone, Apoquel®, Cyclosporine and Cytopoint® is the only possible therapy plan.
Rocky was treated with Apoquel® 16 mg 3/4 tablet every 24 hours (every 12h during the first 14 days). Besides, 1ml of Cortavance® spray (hydrocortisone aceponate) was applied weekly to both ears and also to the skin as proactive therapy.
Although possible skin atrophy with Cortavance® is significantly less likely than with other corticosteroids, the skin should be monitored regularly.
Shampoo therapy was prescribed 1-2 times a week, and Bravecto® every three months was recommended.
To protecting the skin barrier, topical essential fatty acids (EFAs) were applied after the baths. The pruritus was under control with a level between 1-3 out of 10. Periodic rechecks were carried out at least every three months to assess the course of the disease, and the possible appearance of secondary infections.
Discussion
ALD is a pruritic inflammatory skin disease with the same clinical signs as atopic dermatitis, however no allergen-specific IgE against environmental allergens are identified in serology, and the IDT also does not react.
This condition has been known in human medicine for a long time. Atopic dermatitis in human medicine has been divided into intrinsic atopic dermatitis (IAD) and extrinsic atopic dermatitis (EAD). Like dogs with ALD, IAD patients do not show any IgE in serology tests or reaction in the prick test. The prevalence of IAD in human medicine is 10- 45% of cases, that of ALD is described in veterinary literature as 14-25%. Due to the lack of allergen-specific IgE positivity, it is not possible to formulate ASIT in these patients. In the human medical literature, it has been reported that IAD patients can produce allergen specific IgE at a later point in time, but this is still unclear in veterinary medicine. It is therefore uncertain whether it really would make sense to repeat the test at a later point in time.
Rocky showed an excellent response to anti-pruritic treatment (glucocorticoids, oclacitinib, Lokivetmab). There is no clear information on which is the most successful therapeutic approach in patients with ALD. Cyclosporine (CsA) has shown good efficacy in two studies and not shown a good success rate in other reports. To date, no studies have been published about the effectiveness of other drugs in ALD. Little is known about ALD in veterinary medicine, and the diagnosis can be challenging for veterinarians.
In patients with negative allergy test results, it is essential to rule out other pruritic dermatoses such as ectoparasites, food allergy, flea saliva allergy and to adhere to the withdrawal period from medication such as, e.g. Glucocorticoids. Not knowing previous treatments, incorrect test timing or insufficient waiting times for medication are the most common causes of negative allergen test results, which can lead to an over diagnosis of ALD. Therefore, an accurate medical history and proper dermatological examination are needed to avoid incorrect diagnosis.
Amir Davoodi