Goliat is a male dachshund crossbreed born in 2012 (Fig. 5). At the age of 4 years, he was adopted by a Hungarian animal welfare organisation. At that time, he was in poor nutritional condition, had purulent conjunctivitis as well as various skin lesions which were, however, already healing. Additionally, he suffered from recurrent diarrhoea, partly mixed with blood and mucus. Giardia ELISA was positive, and after treatment with fenbendazole, defaecation normalised. As Goliat’s partner dog is allergic to food, he was also kept on a diet (duck and maize). Despite this, he initially had rare, colicky conditions, which were accompanied by borborygmus and inappetence, and occasionally also vomiting. These attacks became more frequent, and ultimately, these symptoms persisted for several days. Since blood screening, faecal analysis and abdominal ultrasound showed no abnormalities and also changing to a light diet only resulted in slight improvements, Helicobacter PCR was performed from vomitus and it was positive. Although the pathogenicity of Helicobacter spp. in dogs is controversial, treatment was begun with metronidazole, amoxicillin and pantoprazole, and already on the 2nd day after the start of therapy, Goliat showed no clinical signs.
After a few months (at the age of 7 years), Goliat was changed back from the light diet to the diet of the allergic partner dog and developed severe itching in both ears within a few days.
Clinical picture
Both pinnae as well as the ear canal were warm, reddened and thickened. In the ear canal, there was also plenty of brownish cerumen with slight yeast odour. The tympanic membrane was not visible.
Cytological examination
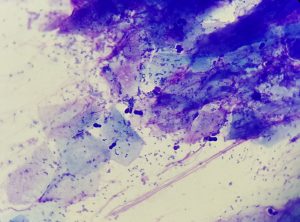
Between the physiologically present keratin debris, the ear swab preparation showed a lot of bacteria (cocci) and also a large number of Malassezia (Fig. 1). In addition to plenty of strands of nuclear material, some intact neutrophil granulocytes were also present.
Initial diagnosis
High-grade septic-purulent otitis externa with Malassezia overgrowth. As otitis externa in dogs is very often caused by food allergies and here, in this case, the temporal connection with the change in diet was striking, the top differential diagnosis was food allergy as the primary disease.
Serological testing for food allergens
The diagnosis “food allergy” is made through an elimination diet which should be carried out for at least 8 weeks, followed by a provocation diet with the previously fed food. If the patient relapses, the food allergy can be diagnosed. The diet can consist of a protein and a carbohydrate source the patient has never eaten before. Because of the vast range of commercial diets available, it is increasingly difficult nowadays to find a diet that has never been fed before.
To select the protein and carbohydrate source for the elimination diet, it is therefore recommended to carry out an allergy test (basic/ extended/exotic food allergy test: for more information see laboklin.com/allergy). Based on the test result, a protein source and a carbohydrate source are selected to which neither IgE nor IgG antibodies react positively. A study of the Small Animal Clinic of the University of Munich showed that the negative predictive value of the food allergy test is 81.1% when both antibody classes are taken into account (Bethlehem et al., 2012). If only components that do not react to IgE and IgG (reaction class zero) are used in the diet, 4 out of 5 dogs are fed a suitable elimination diet. In addition to home-prepared food and commercial high-quality hypoallergenic diets, hydrolysed food can also be used for the elimination diet. Of course, it is necessary to pay attention to good quality and especially to the degree of hydrolysis (peptide size should be < 1 kDa) here as well.
A food allergy test was carried out on Goliat; unfortunately, it showed positive IgE reactions to almost all protein and carbohydrate sources tested and also some positive IgG results. Because of the multi-positive test result, Goliat was now fed a high-quality, hydrolysed diet of poultry feathers (< 1 kDa) and highly purified maize starch (RC Anallergenic®), which his allergic partner dog could also eat.
-
Fig. 1: Ear swab preparation: keratin debris, nuclear fibres (probably from neutrophils) as well as plenty of cocci and some Malassezia
Picture Credits: Dr. Maria Christian
- Fig. 2: Alopecia, erythema and hyperpigmentation medially on the lower foreleg
- Fig. 3: Clearly visible alopecia and hyperpigmentation on the abdomen
- Fig. 4: Seromucous ocular discharge as a result of allergic conjunctivitis
-
Fig. 5: Goliat
Picture Credits: Dr. Maria Christian
Treatment of otitis and food allergy
Unfortunately, it was hardly possible to thoroughly clean the ears or even administer ear drops due to a lack of compliance of the headstrong patient, so that Goliat was given an appointment for ear irrigation under general anaesthesia a few days later. However, even before this detailed examination and treatment, a significant improvement of the signs was noted, which was attributed solely to the change in diet. The swelling had almost completely disappeared and pruritus only manifested itself by an occasional shaking of the head. Thus, after thorough ear cleaning under sedation, no further local therapy was necessary. To avoid having to feed Goliat exclusively with dry food, a wet food version of hydrolysed diet – also based on poultry protein and maize starch (Hill’s z/d®) – was additionally fed after about 6 weeks, when hardly any clinical signs of otitis could be seen. The degree of hydrolysis of this diet was probably insufficient, as otitis externa recurred within a few days. After another change in diet back to solely hydrolysed dry food, otitis was cured again.
One study with dogs allergic to chicken also showed that 40% of patients responded to Hill’s z/d® with significantly increased pruritus, whereas RC Anallergenic® did not cause any worsening of clinical signs in any dog (Bizikova et al., 2016).
Further course
A few weeks later – in early summer – despite strict adherence to the diet, Goliat developed mild pruritus on the ears again, but also on the extremities, in the armpits and on the ventral abdomen. In August, the intensity of pruritus ultimately rose to 8 – 9/10 according to the Pruritus Visual Analogue Scale (PVAS). The skin in these areas showed increasing erythema, moderate alopecia, hyperpigmentation and slight yeast odour (Fig. 2 and 3). Furthermore, moderate, seromucous conjunctivitis was noticed (Fig. 4). As no erosions or crusts were present, a skin impression smear was taken using adhesive tape to check for secondary infections. Microscopically, there was not only plenty of pollen but also accumulations of neutrophil granulocytes as well as cocci and a small number of Malassezia.
The diagnostic assessment of a skin scraping for ectoparasites was not necessary as Goliat had permanently been treated with Simparica® (sarolaner).
Suspected clinical diagnosis
Canine atopic dermatitis (CAD) with secondary infections. Since Goliat was fed exclusively with the highly hydrolysed Anallergenic® diet, it seemed very unlikely that the pruritic symptoms were caused by the food allergy.
Atopy treatment
Goliat was bathed twice a week with a care shampoo containing chlorhexidine (Douxo Pyo®) and, additionally, the skin barrier function was enhanced by essential fatty acids and ceramides. Owing to his strict diet, a spot-on preparation was used (Allerderm®). Although erythema and alopecia improved significantly, pruritus became only slightly better under local therapy. Even a Cytopoint® injection (lokivetmab) could only reduce the itching. Therefore, after taking a blood sample to perform an allergy test for environmental allergens, temporary treatment with prednisolone was started (1 mg/kg per day for 1 week, then 0.5 mg/kg per day).
In combination with regular Cytopoint® injections and continued topical treatment, conjunctivitis was cured after a few weeks and pruritus was improved, but still at a level of 6/10 on the PVAS.
ASIT
Since Goliat had shown a positive reaction in the allergy test to all mites, ASIT was ordered. Prednisolone was tapered before starting desensitisation because in relation to its rather high dosage it did little to improve the pruritic symptoms. ASIT was started according to the treatment plan. Initially, Goliat also got additional Cytopoint® against pruritus. In dogs which do not suffer from pruritus at all after the administration of Cytopoint®, the combination with ASIT would not be recommended, especially at the beginning of treatment. When ASIT is started, it is important that the patients are not completely free of symptoms, because otherwise neither improvement nor worsening of the clinical picture can be seen.
But especially when signs are worsening, it is important to react quickly by adapting the ASIT regimen. As Goliat had never been free of symptoms since the onset of pruritus, Cytopoint® was injected once after the start of ASIT. Even after the end of its duration of action, Goliat did not show any increased itching and after 12 weeks, the only sign of the dog’s allergy were short phases of paw licking, especially in the evening before going to sleep (2 – 3/10 PVAS).
Long-term management
Shampoo therapy was reduced to once a week, the weekly administration of Allerderm® spot-on was continued as well as the permanent administration of Simparica®. Goliat is still fed with RC Anallergenic®. To reduce mite pressure in the environment, every week, all sleeping places are washed at 60 °C and dried in the dryer.
Nevertheless, particularly in late summer, Goliat keeps suffering from phases of increased pruritus. However, so far, these phases could be controlled without the use of systemic anti-pruritic medication by more frequent shampooing and the additional application of skin-calming foam (Douxo Calm®).
This “seasonal” worsening of someone suffering from mite allergy can be explained by the fact that house dust mites can multiply exponentially under certain climatic conditions and, thus, allergen load rises sharply. Another possible explanation could be that Goliat now does show a reaction to pollen from late flowering plants, which was not yet visible in the first allergy test. Therefore, another allergy test on seasonal allergens is planned.
Discussion
CAD affects about 10% of the worldwide dog population and is, hence, a common disease. Depending on the study, 3 – 30% of affected dogs suffer from atopic dermatitis and a food allergy at the same time, as is the case with Goliat.
Pathogenesis of CAD is multifactorial: On the one hand, there is a genetic predisposition, but on the other hand, environmental factors also influence the occurrence and the course of CAD. Some breed predispositions are known (e.g. Labrador, Golden Retriever, WHWT, Bullterrier …) – i.e. Goliat as a mongrel should actually carry a lower risk of developing an allergy.
Environmental factors influencing allergies in dogs have been investigated in various studies, with some of them showing contradictory results. One risk factor identified in almost all studies is living or growing up in an urban environment. The hygiene hypothesis postulated in human medicine, which states that high exposure to microbes in childhood protects against allergic diseases, is also likely to apply to veterinary medicine. Other protective environmental factors are: a rural environment, a lot of time in nature, several animals in the household, home-cooked food during pregnancy and separating puppies late from their mother. Negative risk factors, on the other hand, are a very clean environment and lying on upholstery or in places with a high density of house dust mites. Since nothing is known about Goliat’s early history, to some extent, assessing his risk factors is not possible.
Another risk factor that has recently been studied in human medicine is the use of gastroprotective medication (Jensen-Jarolim et al., 2019). In a large-scale retrospective study, it was shown that especially the use of proton pump inhibitors doubles or triples the risk of allergic symptoms requiring anti-allergic therapy. Not only do the drugs have a direct effect on the immune system, but human medicine has also demonstrated a change in the oral and gastrointestinal microbiome, which creates a pro-allergic environment and promotes the development of allergic diseases. For the past few years, intensive research on the importance of the microbiome has also been conducted in veterinary medicine. First results suggest that the gastrointestinal microbiome may influence the development of obesity, allergic dermatitis and neoplasia as well as cognitive functions and renal function. The development of Goliat’s allergies may have been promoted by the treatment of Helicobacter with pantoprazole.
The case of Goliat shows that not every allergy sufferer responds equally well to the classic treatment options and that an individual, often multimodal management is necessary for each patient. ASIT is an important and effective component of it.
Dr. Maria Christian