(Fig. 1) Pyodermas or bacterial skin infections (Greek: “pyo“ – pus and “derma“ – skin) are highly prevalent in dogs. They are usually secondary to another process or skin disease, so the primary cause must always be investigated in the presence of a pyoderma. There are very different forms of pyoderma depending on the affected area, the depth of the infection or the clinical presentation and each of them receives a specific name. It shows the many faces that skin infection can present and the possible difficulty in its diagnosis.
The traditional classification of pyodermas according to the depth of infection is extremely useful in determining prognosis, therapy and duration of treatment.
Surface pyodermas affect the epidermis and a specific area of the body, e.g. skin folds, interpad, interdigital spaces. They cause pruritus, erythema, exudation, malodour, and even more severe lesions such as erosion and ulceration.
Treatment is based on topical antiseptics and control of pruritus and inflammation where appropriate.
Superficial pyodermas can affect the epidermis, the superficial dermis and the hair follicle. The characteristic lesions of these pyodermas are alopecia, papules, pustules, epidermal collarettes, scaling, scabs and are generally accompanied by pruritus. Treatment requires topical antiseptics and usually topical or systemic antibiotics in addition to the treatment of the primary cause.
Deep pyodermas affect the full thickness of the skin, including the mid and deep dermis and may even affect the panniculus. Lesions are usually painful and include haemorrhagic bullae, nodules, regional swelling, alopecia, ulcers and draining tracts with haemorrhagic, haemopurulent or purulent discharge. Systemic antibiotics are necessary for treatment based on culture and bacterial susceptibility.
The different types of pyodermas and their clinical characteristics are detailed below.
Surface pyoderma:
a. Bacterial overgrowth syndrome is clinically characterised by diffuse erythema, scaling and greasy exudate with whitish or yellowish colour and foul odour. Affected animals are often pruritic. The abdomen, ear pinnae, interdigital and inter-pad spaces are the most commonly affected.
b. Intertrigo or fold pyoderma is caused by fold friction, humidity and temperature, favouring bacterial proliferation. The location of the skin fold accompanies the name affected, e.g.: Intertrigo or pyoderma of facial folds, tail folds, vulvar folds. The affected skin is moist, greasy, erythematous and may contain a whitish malodorous exudate. In severe cases, erosions and ulcerations may occur (Fig. 2).
c. Pyotraumatic dermatitis, hot spot or acute moist pyoderma is produced by a very intense focal pruritic stimulus that causes self-trauma to the area, developing erosive, ulcerative and exudative lesions, and focal alopecia. It is a very acute and severe process that generates not only pruritus but also intense pain in the area. One of the most common primary causes is flea bites.
Diagnosis is based on the clinical picture joinedto cytology results.
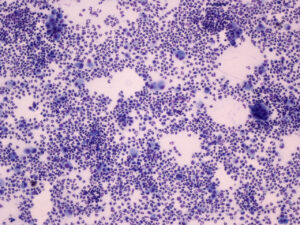
Cytology is characterised by the proliferation of bacteria, usually coccoid and exceptionally bacillary, generally in the absence of inflammatory cells. The presence of inflammatory cells, mainly degenerated neutrophils, usually appears in cases with erosion/ulceration and indicates an intense inflammatory process that should be treated with anti-inflammatory drugs, typically topical corticosteroids. However, some cases may require systemic corticosteroids for a few days, depending on the clinical picture.
Treatment is based on hygiene and the use of antiseptics on the affected area together with topical corticosteroids in case of inflammation. The primary cause must be identified and treated.
Attention: It is not necessary to use antibiotics
-
Fig. 1: The course of lesions in superficial pyoderma is as follows: papules, pustules, crusts, epidermal collarettes and hyperpigmentation
Photo credits: Dr C. Lorente
-
Fig. 2: Facial fold pyoderma (facial intertrigo) in an English bulldog with atopic dermatitis
Photo credits: Dr C. Lorente
-
Fig. 3: Epidermal Collarettes
Photo credits: Dr C. Lorente
-
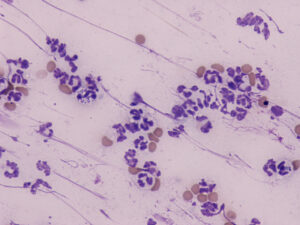
Fig. 4: Note the presence of bacteria (intracellular cocci) inside the neutrophils
Photo credits: Dr C. Lorente
-
Fig. 5: The pyogranulomatous inflammation is shown in cytology by the presence of numerous neutrophils and macrophages
Photo credits: Dr C. Lorente
Superficial pyodermas:
a. Impetigo appears with pustules usually located exclusively on the abdomen of puppies. A similar but severe process can be seen in immunosuppressed older dogs with large flaccid or tense pustules (bullous impetigo).
b. Bacterial folliculitis is the most common form of canine pyoderma and affects the hair follicle producing focal, multifocal or generalised alopecia with the possible presence of papules, pustules, crusts and epidermal collarettes. It is accompanied by itching regardless of the primary cause.
c. Superficial spreading pyoderma is characterised by papules, pustules and epidermal collarettes. Epidermal collarettes can be very large with severe erythema and peripheral exfoliation. The infection causes pruritus in the affected area (Fig. 3).
d. Mucocutaneous pyoderma presents with depigmentation progressing to erosion-ulceration and crusting. It is located in mucocutaneous junctions, mainly on the lips, but it can also appear on the nose, eyelids, vulva, foreskin and anus. Its principal differential diagnoses are discoid lupus erythematosus (DLE) and cutaneous epitheliotrophic lymphoma (CEL), hence the importance of a correct diagnosis since the prognosis and treatment of these three diseases is totally different. Diagnosis is based on clinical presentation and skin biopsy. Prior to biopsy sampling, pretreatment with systemic antibiotics for at least one week is recommended to reduce histopathological lesions associated with a possible secondary bacterial complication in the case of DLE and CEL (Fig. 4).
If pustules are present, diagnosis is based on the clinical presentation and the cytology, in which the presence of bacteria inside the neutrophils will be observed. Cases of bacterial folliculitis without pustules or epidermal collarettes are challenging to diagnose, as only a biopsy can give certainty of diagnosis. The main differential diagnoses of bacterial folliculitis are demodicosis and dermatophytes. So the diagnostic protocol requires trichography to check for the presence of follicular casts (indicating inflammation of the follicle) and the absence of Demodex (ruling out demodicosis), and fungal elements or destruction of the hair shaft structure. If dermatophytosis is the main suspicion, dermatophyte culture or dermatophyte PCR should be performed.
The use of topical antiseptics, preferably in the form of baths, is usually sufficient to treat juvenile impetigo.
The other superficial pyodermas require topical treatment with antiseptics and systemic antibiotic treatment when they are generalised. Localised lesions can respond to antiseptic treatment alone and add topical antibiotics if necessary.
Mucocutaneous pyoderma is a curious process since it requires a very long antibiotic treatment despite being a superficial pyoderma.
Deep pyodermas:
a. Furunculosis. When bacterial infection severely affects the hair follicles, hair follicle rupture or furunculosis occurs. This results in the extension of the infection into the mid and deep dermis and a foreign body reaction associated with the release of hair and keratin into the dermis, producing pyogranulomatous lesions that clinically manifest with nodules, draining tracts, ulcers and crusts.
b. Abscesses are encapsulated collections of pus and necrotic tissue, clinically manifested as erythematous, hot and painful lumps. Usually caused by penetration of bacterial agents through puncture wounds or bites.
c. Cellulitis is diffuse infection and inflammation through tissue planes, usually regional, although it can occur circumscribed. It occurs with swelling, pain and heat. Attention to juvenile cellulitis, which is not an infectious but an immune-mediated process that requires treatment with antiinflammatory/immunosuppressive drugs.
Diagnosis of deep pyodermas is based on the clinical picture, cytology, biopsy and bacterial culture of dermal tissue.
Cytology of furunculosis shows a pyogranulomatous inflammatory reaction due to the foreign body reaction generated by the rupture of hair follicles with mainly neutrophils and macrophages, usually with an eosinophilic component (Fig. 5).
Bacteria are not easily observed within these cytologies. In the case of abscesses, the inflammation is neutrophilic with numerous intra- and extracellular bacteria being observed on cytology examination.
Treatment of deep pyodermas requires the use of systemic antibiotics based on culture and bacterial sensitivity. Abscesses require surgical drainage together with antibiotic therapy.
The duration of antibiotic treatment will depend on the depth of the infection. Superficial pyodermas usually require 3-4 weeks of treatment, deep pyodermas a minimum of 6-8 weeks. Once the clinical cure (complete absence of lesions) has been achieved, treatment should be maintained for a further seven days for superficial infections and at least 14 days for deep infections.
The main bacterial agent in canine pyoderma is Staphylococcus pseudointermedius. Therefore in case of a first episode of non-life-threatening skin infection, with clinical lesions and cytology consistent with superficial pyoderma, where there is no reason to suspect bacterial resistance, treatment with first generation cephalosporins or amoxicillin/clavulanic acid can be selected empirically.
Warning: never use second-line antibiotics (e.g. quinolones) or third-line without a culture and bacterial susceptibility test. Indiscriminate use of antibiotics is negligent and leads to the development of bacterial resistance.
Bacterial culture and sensitivity are necessary whenever any of the following applies:
- Deep pyoderma or life-threatening infections
- No consistency between clinical signs and cytology
- Rod-shaped bacteria on cytology
- Infections not resolving with empirical antibiotic therapy
- Immunosuppressive disease or treatment
- Non-healing wounds
- Post-surgical or nosocomial infections
In general, most pyodermas are secondary to another dermatological or primary systemic disease, which must be investigated, diagnosed and treated to avoid the recurrence of the process. The diseases that most frequently induce the appearance of pyodermas are allergic diseases, it is also common in endocrine disorders such as hypothyroidism and hyperadrenocorticism. But any skin disease can trigger bacterial growth and establish a secondary bacterial infection.
Primary and idiopathic recurrent pyodermas are rare, and their diagnosis is based on ruling out any probable primary disease. Idiopathic recurrent pyoderma often requires prolonged antibiotic therapy and tailored management regimens to prevent recurrences.
Dr Carmen Lorente, DVM, PhD, DipECVD